Es útil revisar algunos conceptos referentes a las heridas fetales y a los factores de crecimiento que empiezan a tener aplicación clínica en úlceras de difícil tratamiento.
Heridas Fetales
En el período fetal, la cicatrización es diferente y se caracteriza por falta de inflamación y de polimorfonucleares, presencia de monocitos y ausencia de contracción y epitelización, en lesiones expuestas al líquido amniótico (103).
Lo más interesante es la inexistencia de cicatriz final, la poca acumulación de colágeno (104, 105) Y los altos niveles de glicosaminoglicanes y ácido hialurónico (106); lo anterior hace pensar más en una estructura en regeneración que en un proceso de reparación.
Las razones para que esto ocurra no son claras, aunque podría ser responsable el medio ambiente fetal con recuentos leucocitarios y niveles de tensión de oxígeno y de factor estabilizante de la fibrina más bajos que en la época posnatal (107, 108). El contacto con el líquido amniótico no parece ser importante (109).
Factores de crecimiento
Son polipéptidos que promueven la proliferación celular actuando sobre receptores externos y que desencadenan cambios intracitoplásmicos que preparan la célula para iniciar la síntesis de ADN Y el proceso mitótico. También facilitan la migración de leucocitos y fibroblastos (110).
Se ha logrado aislar los factores derivados de las plaquetas, y su utilidad en el tratamiento de heridas de evolución tórpida se ha comprobado a través de varios estudios recientes (111-113). Igualmente, se ha demostrado el beneficio de las aplicaciones tópicas del factor de crecimiento epidérmico para acelerar la cicatrización de quemaduras y de áreas donantes de injertos de espesor parcial (114-116).
Miscelanea
La cicatrización es más rápida en ambientes cálidos (300 C) que en fríos (200 C) lo que puede explicarse por la vasoconstricción asociada a estos últimos.
La falta de sensibilidad en el área lesionada suprime este efecto (8), no afecta la contracción ni la epitelización y facilita las ulceraciones por incrementar la colagenólisis ya que la isquemia asociada a presión prolongada disminuye la llegada de alfa-dos macroglobulina del suero que inhibe las colagenasas (117).
Igualmente se ha demostrado un aumento entre el 30 y el 45% de la epitelización y una mayor producción de colágeno si se colocan vendajes oclusivos, quizá por el incremento local de la temperatura (118).
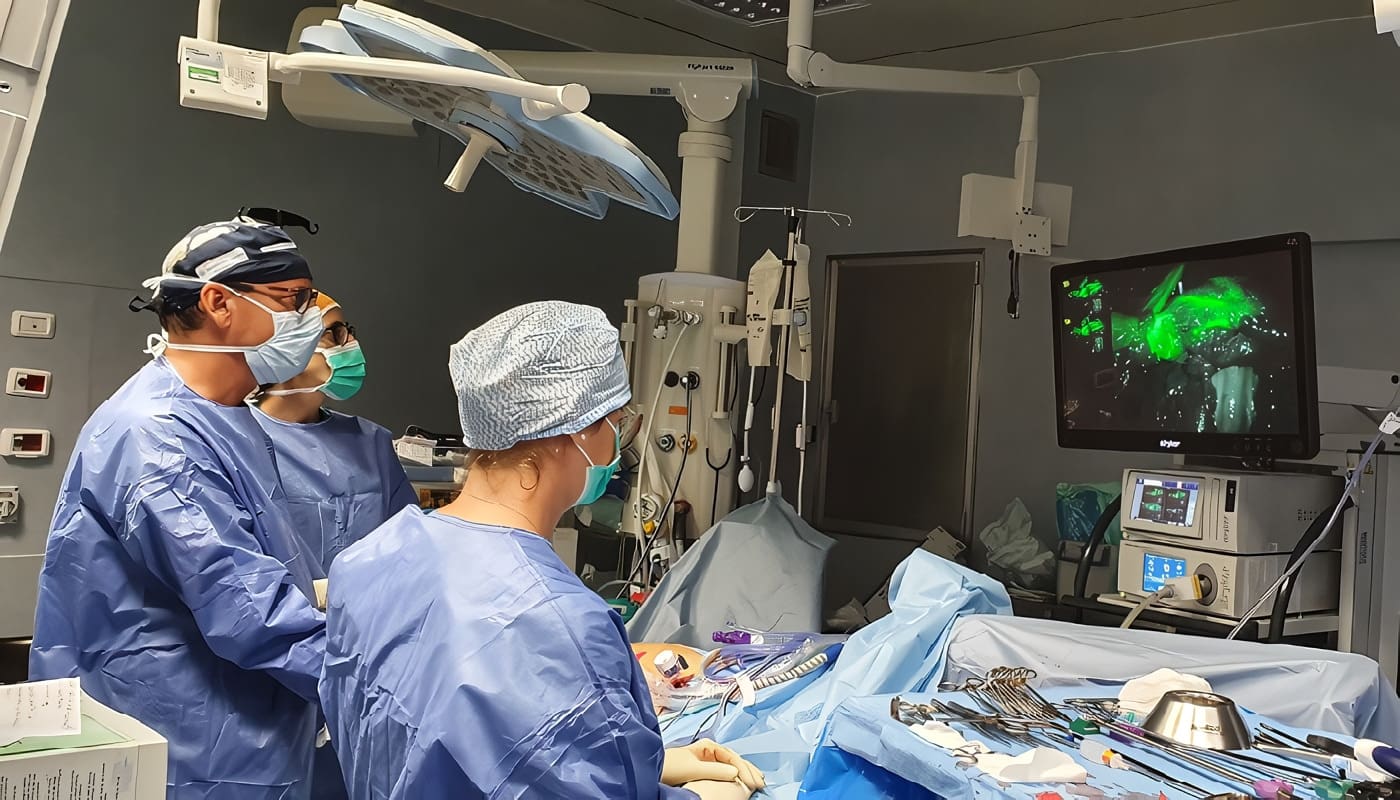
El mecanismo de producción de la herida es un factor interesante en la determinación de la velocidad de los procesos reparativos.
Se observa mayor rapidez cuando no hay infección ni tejido necrótico local, como ocurre en las incisiones quirúrgicas efectuadas con el bisturí convencional.
La utilización de criocirugía, cauterios, ácidos, cáusticos, agentes hemostáticos y láser, retarda en grado variable la cicatrización, puesto que los tejidos desvitalizados deben ser desbridados por la reacción celular antes de iniciar la fibroplasia (119).
Aunque los estudios iniciales con este último demostraron que se favorecía la adherencia de injertos de piel, las investigaciones posteriores comprobaron que se retarda la epitelización y se disminuye la ganancia de fuerza tensil (120).
Hasta el momento no se ha demostrado que el uso de estos instrumentos posea una ventaja real en términos de disminución del tiempo quirúrgico, menor hemorragia o mejor cicatriz, excepto en pacientes con coagulopatías o cuando se realizan procedimientos en áreas excesivamente vascularizadas (121).
El láser de bióxido de carbono no ocluye vasos de calibre mayor de 2 mm y el de argón produce una destrucción tisular biológicamente inaceptable en los bordes de la incisión:
Solamente el de neodimio (Nd: YAG) ofrece algunas ventajas puesto que suprime la producción de colágeno en fibroblastos cultivados y en la piel normal, por lo que podría llegar a ser de utilidad en el tratamiento de queloides (122). Por su parte, los de baja energía, como helioneón (He-Ne) o galio (Ga-As) parecen estimular la fibroplasia in vitro (122).
La aplicación tópica de miel disminuye el edema perilesional, ejerce actividad bactericida, favorece la neovascularización y ayuda al desbridamiento (123). El uso local de factores derivados de plaquetas autólogas estimula la formación de tejido de granulación y acelera la epitelización en algunas ulceraciones crónicas de las extremidades (124).
Es interesante anotar que el envejecimiento fisiológico retarda y prolonga todas las fases reparativas (53, 125) puesto que las mitosis celulares son más escasas, la ganancia de fuerza tensil más lenta y la síntesis de sustancias necesarias para la cicatrización, más pobre. Lea También: Cicatrización y Terapia Inmunosupresora
Abstract
Wound healing is a complex biological process involving several stages wich may be altered by numerous drugs and common diseases.
This article updates current knowledge regarding the different alterations that might be associated with malnourishment and vitamin deficiencies and the nature of the problems observed after radiotherapy. Finally, it reviews some information regarding fetal wound healing and the growth factors that have became available for the treatment of chronic non-healing wounds.
Referencias
- Levenson S M, Seifter E, Van Winkle W Jr: Nutrition. In: Hunt T K, Dunphy J E: Fundamentals of wound managemenl. Apleton- Century-Crofts, New York, 1979 Irvin T T: Effeets of malnutrition and hyperalimentation on wound healing. Surg Gynecol Obstet 1978; 146: 33
- Barbul A, Rellure G, Levenson S M et al: Arginine: A thymotropic and wound healing promoting agent. Surg Forum 1977; 28: 101
- Fitzpatrick D W, Fisher H: Camosine, histidine and wound healing, Surgery 1982; 91: 56
- Ruberg R L: Role of nutrition in wound healing. Surg Clin North Aro 1984; 64: 705
- Windsor J A, Knight G S, HilI G L: Wound healing response in surgical patients: Recent food intake is more important than nutritiona! status. Brit J Surg 1988; 75: 135
- Haydock D A, Hill G L: Improved wound healing response in surgical patients reeeiving intravenous nutrition. Brit J Surg 1987; 74: 320
- Peacock E E Jr: Wound repair. 3a ed., Philadelphia: W. B. Saunders Co., 1984 9. Pollack S V: Systemic medications and wound healing. Int J Dermatol 1982; 21: 489
- Ringsdorf W M Jr, Cheraskin E: Vitamin C and human wound healing. Oral Surg 1982; 53: 231
- Afifi A M, Ellis L, Hunstman R G, Said M 1: High dose ascorbic acid in the management of thalassemia leg ulcers. A pilot study. Bril J Dermalol 1975; 92: 339
- Elsas L J, MilIer R L, Pinell S R: Inherited human collagen Iysyl hydroxylase deficiency: Ascorbic acid response. J Pedialr 1978; 92: 378
- Ehrlich H P, Tarver H, Hunl T K: Inhibitory effeets of vilamin E on collagen synlhesis and wound repair. Ann Surg 1972; 175: 235
Otras Referencias
- Alvarez O M, Gilbreath R L: Effeel ef dielary thiamine on intermoleeular collagen cross-linking during wound repair: A meehanical and biochemical assessmenl. J Trauma 1982; 22: 20
- Kumar M, Axelrod A E: Cellular antibody synlhesis in vilamin B6-deficienl rale. J Nutr 1968; 96: 53
- Aprahamian M, Denlinger A, Stock- Damgé C, Kovassi J C, Grenier J F: Efecls of suplemental panlothenic acid on wound healing: Experimental sludy in rabbits. Am J Clin Nulr 1985; 41: 578
- Ninikoski J: Tbe effecl of blood and oxygen supply on the biochemeslry of repair . In: Hunt T K: Wound healing and wound infeclion: Tbeory and surgical praclice. Appleton-Century-Crofts, New York,1980
- Hunl T K, Pai M P: Tbe effeet of varying ambienl oxygen tensions on wound metabolism and collagen synthesis. Surg Gynecol Obstel 1972; 135: 561
- Carrico T J, Mehrhof Al Jr, Cohen I K: Biology of wound healing. Surg Clin Norlh Am 1984; 64: 721
- Miller T A: Tbe healing of parlial-thickness skin injuries. In: Hunt T K: Wound healing and wound in fections: Tbeory and surgical praclice. Applelon-Century-Crofts, New York, 1980
- Hunl T K: Disorders of repair and Iheir management. In: Hunl T K, Dunphy J E: Fundamenlals of wound managemenl. Applelon- Century-Crofts, New York, 1979
- Hart G, Mainous E G: Tbe trealment of radiation necrosis wilh hyperbaric oxygen (OHP). Cancer 1976; 37: 2580
- Davis J C, Dunn J M, Gales G, Heimbach R D: Hyperbaric oxygen: A New adjunt in Ihe managemenl of radialion necrosis. Arch Oto laryngo I 1979; 105: 58
- Perrins D J D: Hyperbaric oxygen and skin coverage. HBO Rev 1983; 4: 179 25. Slack W 1, Tbomas D A, Perrins D: Hyperbaric oxygenation in chronic osteomyelilis. Lancel 1: 1093-965.
Bibliografías
- Goddio A S: Oxygen derived free radicals in plastic surgery- Tberapeulic inleresl of fighting free radicals: Tbe superoxide dismutases. Eur J Plast Surg 1989; 12: 111
- Heughan C, Chir B, Grislis G, Hunl T K: Tbe effeet of anemia on wound healing. Ann Surg 1974; 179: 163
- Jensen J A, Goodson W H I1I, Vasconez L O, Hunt T K: Wound healing in anemia. West J Med 1986; 144: 465
- Taylor D E M, Whamond J S, Penhallow J E: Effects if hemorrhage on wound strength and fibroblast function. Brit J Surg 1987; 74: 316
- Berlinger N T: Wound healing. Otolaryngol Clin North Am 1982; 15: 29
- Chvapil M: Zinc and other factors of the pharmacology of wound. In: Hunt T K: Wound healing and wound infection: Theory and surgical practice. Appleton-Century-Crofts, New York, 1980
- Mertz W: Chromium and its relation lo carbohydrate metabolism. Med Clin North Am 1976; 60: 739
- Schwartz K: Essentiality and metabolic functions of selenium. Med Clin North Am 1976; 60: 745
- Hunt T K, Van Winkle W Jr: Normal repair In: Hunt T K, Dunphy J E: Fundamentals of wound management Appleton- Century- Crofts, New York, 1979
- O’Hare R P, Fallon A, Bradley J F, Burns J, McGee J O D: lsolation of collagen stimulating factor s from healing wounds. J Clin Pathol 1983; 36: 707
- Ahonen J, Jiborn H, Zeberfeldt B: Hormone intluence on wound healing. In: Hunt T K: Wound healing and wound infeetion: Theory and surgical practice. Appleton-Century-Crofts, New York, 1980
Otras Bibliografías
- Uino J, Mustakallio K K: Effect of hydrocortisone acetate, tluoclorolone acetonide, betamethasone-17 valerate and f1uprednyliden acetate on collagen biosynthesis. Biochem Pharmacol 1971; 20: 2495
- Dykes P J, Marks R: An appraisal of the methods used in the assessment of atrophy from topical corticosteroids. Brt J DermatoI1979; 101: 599
- Sandberg N: Time relationship between administration of cortisone and wound healing in rals. Acta Chir Scand 1964; 127: 446
- Salmela K, Abonen J: The effect of methylprednisolone and vitamin A on wound healing. Acta Chir Scand 1981; 147: 307
- Salmela K: The effect of methylprednisolone and vitamin A on wound healing. Acta Chir Scand 1981; 147: 313 Micksche M, Cerni C, Kokron O,
- Titscher R. Wrba H: Stimulation of immune response in lung cancer patients by vitamin A therapy. Oncology 1977; 34: 234
- Cohen B K, Gill G, Cullen P R, Morris P J: Reversal of postoperative immunosupresion in man by vitamin A. Surg Gynecol Obstet 1979; 149: 658
- AlIen H 1.., Wase A, Bear W T: Indomethacin and aspirin: Effect of nonsteroidal anti-inflammatory agents on the rate of fracture repair in the ra!. Acta Orthop Scand 1980; 51: 595
- Carlstedt C A: Mechanical and chemical factors in tendon healing. Effeets of indomethacin and surgery in the rabbit. Acta Orthop Scand (Suppl) 1987; 224: 52
- Bateman B G, Nunely W C, Kitchins J D: Prevention of postoperative peritoneal adhesions: An assessment of ibuprofen. Am CoII Surg Forum 1981; 21: 603
- Siegel A M, Kontopulus V, Wang C F: Prevention of postoperative adhesions in rabbits with ibuprofen, a nonsteroidal anti-intlamarory agent. Fertil Steril 1980; 34: 46
Fuentes
- Kulick A, Michael 1, Smith S, Hadler K: Oral ibuprofen: Evaluation of its effeet on peritendinous adhesions and the breaking of a tenorrhaphy. J Hand Surg 1986; 11A: 110
- Alvarez O M, Levendorf D D, Smerbeck R V et al: Effeet of topically applied steroidal and nosteroidal anti-intlamatory agents on skin repair and regeneration. Fed Proc 1984; 43: 2793
- Kozol R A, Gillies C, Elgebaly S A: Effects of sodium hypochlorite (Dakin’s solution) on ce lis of the wound module. Arch Surg 1988; 123: 420
- Lineaweaver W, McMorris S, Soucy D, Howard R: Cellular and bacterial toxicities of topical antimicrobials. Plast Reconstr Surg 1985; 75: 394
- Branemark P 1, Ekholm R, Albrektsson B et al: Tissue injury caused by wound disinfectants. J Bone Joint Surg 1967; 49A: 48
- Goslen J B: Physiology of wound heal· ing and scar formation. In: Thomas J R, Holt G R: Facial scars: Incision, revision and camoutlage. St. Louis: C. V. Mosby CO., 1989
- Ferhat S M, Amer N S, Weeks D S, Musselman M M: Effect of mechlorthamine hydrochloride (nitrogen mustard) in healing of abdominal wounds. Arch Surg 1958; 76: 749
- Desprez J D, Kiehn C L: The effects of cytoxan (cyclophosphamide) on wound healing. Plast Reconstr Surg 1960; 26: 301
- Smith R W, Sampson M K, Lucas C E et al: Effects of vinblastine, etoposide, cisplatin and bleomycin on rodent wound healing. Surg Gynecol Obstec 1985; 161: 323
- Lawrence W T, Talbot T 1.., Norton J A: Preoperative or postoperative doxorubicin hydrochloride (adriamycin): Which is bener for wound healing? Surgery 1986; 100: 9
- Ferguson M K: The effect of antineoplastic agents on wound healing. Surg Gynecol Obstet 1982; 154: 421
Otras Fuentes
- Moynahan E J: Penicillamin in the treat· ment of morphea and keloids in children. Postgr Med J 1974 Aug (Suppl); 39
- Peacock E E Jr: Pharmacological control of surface scarring in human beings. Ann Surg 1981; 193: 592
- Peacock E E Jr: Control of wound healing and scar formation in surgical patients. Arch Surg 1981; 116: 1325 62. Borden E B, Sammartano R J, Dembe C, Boley S J: The effect of metronidazole on wound healing in rats. Surgery 1985; 97: 331
- Scher K S, Scon-Conner C E H: Detrimental effect of a cephalosporin on early fascial healing. Surg Forum 1986; 37: 116
- Zimmerman A, Truss F: The effect of antibiotic drugs on wound healing. Urol Res 1974; 2: 73
- Scher K S, Scott-Conner C E H, Montany P F: Effect of cephalosporins on fascial healing after celiotomy. Am J Surg 1988; 155: 361
- Morris T, Tracey J: Lignocaine: Its effeet on wound healing. Brit J Surg 1977; 64: 902
- Eichhorn J H, Peterkofsky B: Local anesthetic-induced inhibition of collagen secretion in cultured cells under conditions where microtubules are not depolyrnerized by these agents. J Cell Biol 1979; 81: 26 68. Morris T, Appleby R: Retardation of wound healing by procaine. Brit J Surg 1980; 67: 391
- Edlich R F, Rodeheaver G, Thacker J G, Edgerton M T: Technical factors in wound management. In: Hunt T K, Dunphy J E: Fundamentals of wound management. Appleton-Century-Crofts, New York, 1979
- Stevenson T R, Rodeheaver G T, Goldern G T: Damage to tissue defenses by vasocontrictors. J Am CoII Emer Phys 1975; 4: 532
- Edlich R F, Rodeheaver G T, Kurtz L et al: Treatise on the contaminated wound. In: Krizek T J, Hoopes J E: Syrnposium on basic science in plastic surgery.St Louis: C, V. Mosby Co., 1972
Lecturas Recomendadas
- Tran D T, Miller S H, Buck D et al: Potentiation of infection by epinephrine. Plast Reconstr Surg 1985; 76: 933
- Alvarez O M, luzzolino A, O’Hare W, Gilbreath R L: Testosterone increases collagen deposition in experimentally induced granulation tissue. Fed Proc 1981; 40: 343
- Rojkind M, Uribe M, Kershenobich D: Colchicine and the treatment of liver cirrhosis. Lancet 1973; 1: 38
- Dubrawsky C, Dubrawsky N B, Withers H R: The effect of colchicine on the accumulation of hydroxyproline and on the lung compliance after irradiation. Radiat Res 1978; 73: 111
- Simpson G, Kunz E, Slafta J: Use of sodium dyphenylhydantoin in treatment of leg ulcers. N Y J Med 1965; 65: 886
- Brinckerhoff C E, McMillan R M, Dayer J M, Harris E D: Inhibition by retinoic acid of collagenase production in rheumatoid synovial cells. N Engl J Med 1980; 303: 432
- Hung V C, Yu-Yun Lee J, Zitelli J A, Hebda P A: Topical retinoin and epithelial wound healing. Arch Dermatol 1989; 125: 65
- Arumugam S, Ninmannit S, Enquist I F: The effect of immunosuppression on wound healing. Surg Gynecol Obstet 1971; 133: 72
- Nemlander A, Abonen J, Wiktorowicz K et al: Effect of cyclosporine on wound healing. An analysis with viscous cellulose sponges. Transplantation 1983; 36: 1
- Eisinger D R, Ross Shell A G: A comparison of the effects of cyclosporin A and standard agents on primary wound healing in the rato Surg Gynecol Obstet 1985; 160: 135
- Hinz J, Hautzinger H, Stahl K W: Rationale for and results from a randomized double-blind trial of tetrachlorodecaoxygen anion complex in wound healing. Lancet 1986; 1: 825 83. Hatz R A, Kelley S F, Ehrlich P E: Tbe tetrachlorodecaoxygen complex reverses the effect of cortisone on wound healing. Plast Reconstr Surg 1989; 84: 953
Otras Lecturas Recomendadas
- Goodson W H I1I, Radolf J, Hunt T K: Wound healing and diabetes. In: Hunt T K: Wound healing and wound infection: Theory and surgical practice. New York, Appleton-Century-Crofts, 1980
- Seifter E, Rettura G, Padawer J et al: Impaired wound healing in streptozocin diabetes. Prevention by supplemental vitamin A. Ano Surg 1981; 194: 42
- Mosely L H, Finseth F, Goody M: Nicoline and its effecl on wound healing. Plast Reconslr Surg 1978; 61: 570
- Lawrence W T, Murphey R C, Robson M C el al: Tbe delrimenlal effecl of cigarette smoking on flap survival: Ann experimental sludy in the ra!. Bril J Plasl Surg 1984; 37: 216
- Benvenisle K, Thut P: Tbe effect of chronic alchoholism on wound healing. Proc Soc Exp Biol Med 1981; 166: 568
- Buknall T E: Tbe effect of local infeclion upon wound healing: An experimental study. Brit J Surg 1980; 67: 851
- Robson M C, Slenberg B D, Heggers J P: Wound healing a1terations caused by infeclion. Clin Plast Surg 1990; 17: 485
- Colin J F, Elliol P, Ellis H: The effect of uremia upon wound healing: An experimenlal study. Brit J Surg 1979; 66: 793
- Grinell F, Billingham R E, Burgess L: Distribution of fibronectin during wound healing in vivo. J Invest Dermatol 1981; 76: 181
- Repesh L A, Fitzgerald T J, Furchl L T: Fibronectin involvement in granulation tissue and wound healing in rabbits. J Histochem Cytochem 1982; 30: 351
- Hulsey T K, O’Neill J A, NebblettWR, Meng H C: Experimental wound healing in essenlial fatty acid deficiency. J Pedialr Surg 1980; 15: 505
Referencias Bibliográficas
- Uitto J, Tan E M L, Ryhanen L: Inhibition of collagen accumulation in fibrotic processes: Review of pharmacological agents and new approaches with amino acids and their analogues. J Invest DermaloI1982; 79: 113
- Bayer 1, Ellis H: Jaundice and wound healing: Ano experimental study. Bril J Surg 1976; 63: 392
- Amstrong C P, Dixon J M, Duffy S W et al: Wound healing in obslructive jaundice. Bril J Surg 1984; 71: 267
- Askew A R, Bates G J, Balderson G: Jaundice and the effect of sodium taurocholate taken orally upon abdominal wound healing. Surg Gynecol Obstet 1984; 159: 207
- Viljoen D L, Bloch C, Beighton P: Plaslic surgery in pseudoxanthoma elas- ‘ ticum: Experience in nine patients. Plast Reconslr Surg 1990; 85, 233
- Levenson S M, Gruber C A, Rettura G et al: Supplemental vitamin A prevents the acute radiation-induced defect in wound healing. Ann Surg 1984; 200: 494
- Mustoe T A, Purdy J, Gramates P et al: Reversal of impaired wound healing in irradiated rats by plateletderived growth factor-BB. Am J Surg 1989; 158: 345
- Taren D L: Increasing the breaking strength or wounds exposed to preoperative irradiation using vitamin E supplementalion. Int J Nutr Res 1987; 57: 133
- Rowlatt U: Intrauterine wound healing in a 20-week human fetus. Virchows Arch [A] 1979; 381: 353
- Robinson B W, Goss A N: Instrauterine healing of fetal rat cheek wounds. Cleft Palate J 1981; 18: 251
- Hallock G G, Rice D C, McClore H M: In utero Iip repair in the rhesus monkey. Plast Reconstr Surg 1987; 80: 855
Otras Referencias Bibliográficas
- Krummel T M, Nelson J M, Diegelmann R F et al: Fetal response to injury in the rabbit. J Pediatr Surg 1987; 7: 640
- Playfair J H L, Wolfendale M R, Key H E M: The leukocytes of peripheral blood in the human fetus. Bril J. Haematol 1963; 9: 336
- Chignier E, Baguet J, Dessapl B et al: Skin healing and fibrin stabilizing factor levels in the rabbit fetus. J Surg Res 1981; 31: 415
- Sullivan W G: In utero cleft Iip repair in the mouse without an incision. Plast Reconstr Surg 1989; 84: 723
- McGralh M H: Peptide growth factors and wound healing. Clin Plast Surg 1990; 17: 421
- Doucette M M, Fylling C P, Knighton D R: Prevention of lower extremity amputation due to nonhealing wounds in a high-risk population: Use of plalelet derived wound healing formula and a defined wound care protocol. Arch Phys Med Rehabil 1989; 70: 780
- Knighton D R, Ciresi K F, Fiegel V D et al: Slimulation of repair in chronic nonhealing cutaneous ulcers: A prospeclively randomized blinded trial using platelet-derived wound healing formula. Surg Gynecol Obstet 1990; 170: 56
- Fylling C P, Knighton D R, Gordinier R: Tbe use of a comprehensive wound care protocol including topical growth factor lherapy in treatment of diabelic plantar ulcers. In: Ward J: Diabetic neuropathy, Wiley, Chicherter, U. K., 1990
- Brown G L, Schultz G, Brightwee J R, Tobin G R: Epidermal growth factor enhances epilhelializalion. Surg Forum 1984; 35: 565
- Brown G 1, Curtsinger L, Brightwell J R, Ackerman D M: Enhancement of epidermal regeneration by biosynthetic epidermal growth factor. J Exp Med 1986; 163: 1319
- Brown G L, Nanney L B, Griffen J el al : Enhanccement of wound healing by topical lreatment with epidermal growth factor. N Engl J Med 1989; 321: 76
Fuentes Bibliográficas
- Basson M D, Bumey R F: Defective wound healing in patients with paraplegia and quadriplegia. Surg Gynecol Obstet 1980; 155: 9
- Alvarez O M, Mertz P M, Eaglstein W H: Tbe effect of occlusive dressings on collagen synthesis and reepithelialization in superficial wounds. J Surg Res 1983; 35: 142
- Zitelli J: Wound healing for clinician. Adv Dermatol 1987; 2: 243
- Sowa D, Masterson B J, Nealon N, Von Fraunhofer J A: Effects of thermal knives on wound healing. Obstet Gynecol 1985; 66: 436
- Wieman T J: Lasers and the surgeon. Am J Surg 1986; 151: 493
- Abergel R P, Meeker C A, Lam T S: Control of connective tissue metabolism by lasers: Recent developments and future prospects. J Am Acad Dermatol 1984; 11: 1142
- Efem S E E: Clinical observations on the wound healing properties of honey. Brit J Surg 1988; 75: 679
- Knighton D R, Ciresi K F, Fiegel V D et al: Classification and treatment of chronic nonhealing wounds. Successful treatment with autologous plateletderived wound healing factors. Ann Surg 1986; 204: 322
- Eaglstein W H: Wound healing and aging. Dermatol Clin 1986; 4: 481
SOCIEDAD COLOMBIANA DE CIRUGÍA
XVII Congreso Nacional
“Avances en Cirugía”
” HOTEL TEQUENDAMA “
14, 15, 16 Y 17 de agosto de 1991
Conferencistas invitados
- Doctor Luis Eduardo Cortés – Estados Unidos
- Doctor Lemuel Herrera – Estados Unidos
- Doctor Enrique Moreno – España
- Doctor Raúl Praderi – Uruguay
- Doctor Aurelio Rodríguez – Estados Unidos
Habrá presentación de “Trabajos Libres”. Quienes deseen participar en ellos, deberán enviar el respectivo resumen a la sede de la SOCIEDAD antes del 15 de junio de 1991.
Igualmente se realizarán “Almuerzos de Trabajo” con temas de interés para los asistentes.
Informes e inscripción de trabajos: Calle 100 ND 14 – 63, Of. ND 502 – Tel: 257-4560 y Telefax 257-4501. Bogotá, D.E., Colombia.
Doctor Alberto Kurzer Schan Jefe de la Secc. de Cirugía Plástica, Maxilofacial y de la Mano, U. de Antioquia, Hosp. Univ. San Vicente de Paúl Medellín, Colombia.