Conclusiones
Al finalizar este trabajo se pudo concluir que:
- La inmunoterapia sublingual-oral ofrece seguridad y efectividad en el tratamiento del paciente alérgico.
- Todos los pacientes que hicieron correctamente el tratamiento siguiendo las instrucciones pre-establecidas obtuvieron mejoría de su enfermedad alérgica al terminar el estudio.
- No fue posible discriminar en cuanto a las diferentes enfermedades alérgicas tratadas y la respuesta al tratamiento, pues todas respondieron con cese de signos y síntomas antes de los dos meses de iniciado el tratamiento y sin importar el tiempo de evolución de la enfermedad.
- El tiempo empleado en el tratamiento ( 6 meses) es considerablemente corto. Únicamente en dos niños hubo necesidad de prolongar a un año la administración de las gotas sublinguales
- Resaltamos el hecho de que aunque el tiempo de tratamiento establecido es de 6 meses algunos pacientes (niños) suspendieron el tratamiento en períodos de tiempo mas cortos pero igualmente se encuentran en remisión de su enfermedad alérgica.
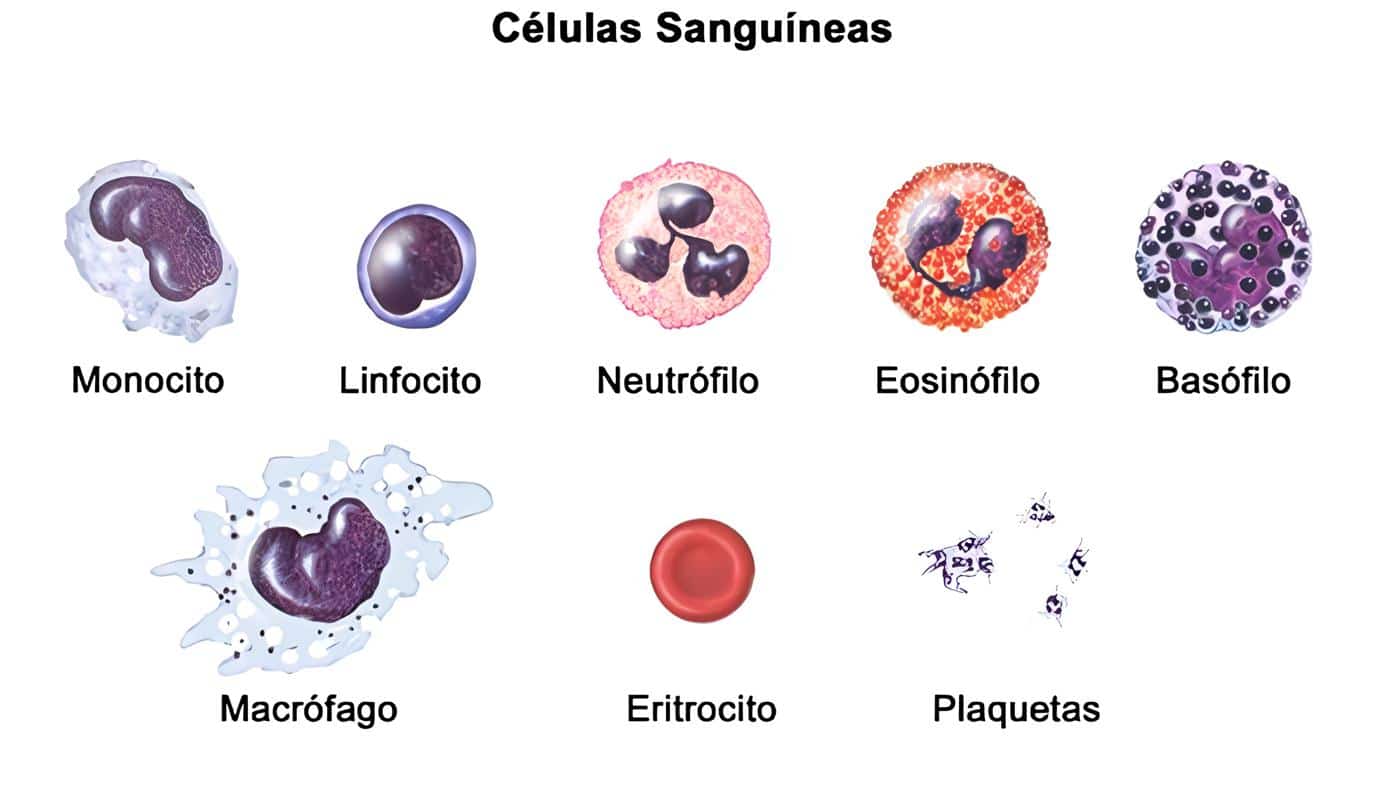
- Desde el punto de vista paraclínico se encontró una marcada respuesta humoral por inmunoglobulina A secretora en más del 80% de los pacientes, como anticuerpo neutralizante del alergeno en cuestión.
- La inmunoglobulina E que en todos los pacientes tenía títulos elevados al iniciar el tratamiento, tuvo un comportamiento irregular pues sólo un 33 % normalizó sus títulos y por el contrario un 67% permaneció igual o aumentó los títulos de este anticuerpo.
- Como efecto colateral al iniciar el tratamiento se manifestó en un paciente un intenso prurito en garganta yen otro una conjuntivitis muy pruriginosa, en ambos casos remitió el síntoma al indicarle al paciente que no deglutiera el alergeno sino que lo escupiera después de sostenerlo debajo de la lengua por 3 minutos.
- En cuanto a recaídas de la enfermedad después del tratamiento es muy temprano para saber cómo se comportará la enfermedad después de suspendido el tratamiento pues el paciente más antiguo tiene 1 año 7 meses de observación asintomático. Un paciente hizo recaída leve de asma bronquial al año, la cual cedió al reforzar la inmunoterapia con alergenos puros durante 1 mes.
- En dos pacientes fue necesario llevar al doble la dilución de los alergenos administrados, pues con las diluciones preestablecidas (Gráfica 1) presentaron agudización de los síntomas de su enfermedad (asma bronquial en ambos casos).
- El procedimiento fue más dispendioso en niños debido al sabor de los alergenos y debido a esto hubo necesidad de suspender el tratamiento en algunos casos antes de cumplir con el tiempo preestablecido.
Referencias Bibliográfica
- Van Hoogstraten IM, Burrows D, Camarasa JG, Domos Goossens A, Kraal G; Latí A, et al. Reduced frecuency of nickel allergy upon oral nickel contact at an early age. Department of Pathology Free University Amsterdam, The Netherlands. Clin Exp Immunol 1991; 85 (3):441-5.
- Meaga J, Fugihashi K, Yamamoto M, McGhee JR, et al. Cytokine production and T cell receptor expression by salivary glands T cells and intraepithelial T lymphocites for the regulation of the Ig A response. Department of oral Biology, University of Alabama, Birminham. Adv Exp Med Biol 1992; 327: 119- 31.
- Brandtzaeg P, Halstensen TS, Huitfeldt Hs, Krajci F, Kvale D, Scott H, Thrane PS. Epithelial expression of HLA, secretory component (poly Ig.) Receptor, and adhesion molecules in the human alimentary tract. Laboratory for Immunohistochemistry and Immunopathology (LIIPAT),University of Oslo, National Hospital, Rikshospitalat, Norway. Ann N Y Acad Scl 1992; 664;157-79.
- Van-Hoogstraten IM, Bodenj D, Vonj Blomberg ME, Kraal G, Scheper RJ. Persistent immune tolerance to nickel and chromium by oral administration prior to cutaneous sensitization. Department of Pathology, Viraje University, Amsterdam, The Netherlands. J Invest Dermatol 1992 Nov; 99(5): 6º8-16.
- Revillard JP, Cozon G, Czerkinski C. Oral administration of immunomodulators and the mucosal immune system. Laboratoire d’Immunologie, INSERM U80 CNRS URA 1177 UCBL.Hôpital E. Herriot, Lyon, France. Dev Biol Stand 1992; 77: 31-7.
- Tlaskalova Hogenova H, Mandel L, Stepankova R, et al. Autoimmunity: from physicology to pathology. Natural antibodies, mucosal immunity and development of B cell repertoire. Division of Immunology and Gnotobiology, Czehoslovak Academy of Sciences, Praha. Folia Biol Praha 1992; 38 (3-4): 202-15.
- Fujihashi K, Taguchi T, Aicher WK, McGhee JR, et al. Immunoregulatory functions for murine intraepithelial lymphocytes: gamma/delta T Cell receptor – Positive (TCR+) T Cells abrogate oral tolerance, while alpha/beta TRC + T Cells provide B Cell help. Departament of Oral Bíology, University of Alabama, Birmingham 35294. J Exp Med 1992 Mar 1; 175 (3): 695-707.
- Gonzalez Ariki S, Lopez MC, Roux ME. IgA B lymphocytes and subpopulations of T lymphocytes in the Intestinal villi of immunodeficient wistar rats. Departament of Biological Sciences, Faculty of Pharmacy and Biochemistry, Buenos Aire University, Argentina. Reg Immunol 1992 Jan- Feb; 4 (1): 41-5.
- Kagnoff MF. Immunology of the intestinal tract. Departaments of Medicine, University of California, San Diego, La Jolla. Gastroenterology 1993 Nov; 105 (5): 1275-80.
- Laissue JA, Chappuis BB, Muller C, Reubi JC, Gebbers JO. The intestinal immune system and relation to disease. Institute of Pathology, University of Bern, Switzerland. Dig Dis 1993 Jul-Oct; 11 (4-5): 298-312.
- Van Hoogstraten IM, Boos C, Boden D, Von Blomberg ME, Scheper RJ, Kraal G. Oral induction of tolerance to nickel sensitization in mice. Departament of pathology, Vrije Universiteit, Amsterdam, the Netherlands. J Invest Dermatol 1993 Jul; 101 (1): 26-31.
- Kim SM, Enomoto A, Hachimura S, Yamauchi K, Kaminogawa S. Serum antibody response elicted by a casein diet is directed to only limited determinants of alpha Sl- Casein. Departament of Agricultural Chemistry, University of Tokyo, Japan. Int Arch Allergy Immunol 1993; 101 (3): 260-5.
- Blumberg RS, Yockey CE, Gross GG, Ebeet EC, Balk SP. Human intestinal intraepithelial lymphocytes are derived from a limited number of T cell clones that utilize multiple V beta T Cell receptor genes. Gastroenterology Division, Brigham and women’ s Hospital, Harvard Medical School, Boston, MA 02115.J Immunol 1993 Jun 1; 5144- 53.
- Hoyne GF, Callow MG, Kuhlman J, Thomas WR. T cell lymphokine response to orally administered proteins during priming and unresponsiveness. Division of Molecular Biology, Western Australian Research Institute for Child Health, Princess Margaret Hospital, Perth. Immunology 1993 Apr; 78 (4): 534- 40.
- Liu LM, Macpherson GG. Antigen acquisition by dendritic cell: intestinal dendritic cell acquire antigen administered orally and can prime naive T cell in vivo. Sir william Dunn School of Pathology, University of Oxford, Unted Kingdom. J Exp Med. 1993 May 1; 177 (5): 1299- 307.
- Melamed D, Friendman A. Direct evidence for anergy in T lymphocytes tolerized by oral administration of ovalbumin. Departament of Animal Science, Hebrew University of Jesusalem, Rehovot, Israel. Eur J Immunol 1993 Apr; 23 (4): 935- 42.
- Faria AM, Garcia G, Rios MJ, Michalaros CL, Vaz NM. Decrease in susceptibility to oral tolerance induction and occurrence of oral immunizationm to ovalbumin in 20- 38- week- old mice. The effect of interval beetween oral exposures and rate of antigen intake in the oral immunization. Departamento de Microbiologia, Instituto deCiencias Biologicas, UFMG, Belo Horizonte. Brasil. Immunology 1993 Jan 78 (1): 147-51.
- Kaminogawa S, Hisatsune T, Hachimura S. (The molecular biology of oral tolerance). Departament of applied Biological Chemistry, University of Tokyo, Japan. Tanpakushitsu- Kakusan- Koso. 1994 Sep; 39 (12); 2090-101.
- Aramaki Y, Fuji Y, Suda H, Suzuki I, Yadomae T, Tsuchiya S. Induction of oral tolerance after feeding of ragweed pollen extract in mice. Tokyo Collage of pharmacy, Japan. Immunol Lett 1994 Apr; 40 (1): 21- 5.
- Friedman A, Weiner HL. Induction of anergy or active suppression following oral tolerance is determined by antigen dosage. Center for Neurologic Diseases, Brigham and women‘s Hospital, Harvard Medical school. Boston, MA 02115. Proc Natl Acad Sci U S A 1994 Jul 5; 91 (14): 6688- 92.
- Miller BG, Whittemore CT, Stokes CR, Telemo E. The effect of delayed wening on the development of oral tolerance to soya- bean protein in pigs. School f Veterinary Science, Bristol University, Langford. Br J Nutr 1994; 71(4): 615-25.
- Weiner HL, Friedman A, Miller A, Khoury SJ, Al Sabbagh A, Santos L. Oral tolerance: immunologic mechanisms and treatment of animal and human antigens. Center for Neurologic Diseases, Brigham and women‘s Hospital, Boston, Massachusetts. Annu Rev Immunol 1994; 12: 809- 37.
- Friedman A, Al Sabbagh A, Santos LM, et al. Oral tolerance: a biologically relevant pathway to generate peripheral tolerance external and self antigens. Center for Neurological Diseases, Brigham and women‘s Hospital, Boston, Mass. Chem Immunol 1994; 58: 259- 90.
- Carvalho CR, Verdolin BA, De Souza AV NM. Indirect effects of Oral tolerance in mice Instituto de Ciencias Biologicas, Universidade Federal de Minas Gerais Belo Horizonte, Brasil Scand J Immunol 1994 Jun; 39 (6): 533- 8.
- Hancock WW, Khoury SJ, Carpenter CB, Sayegh MH. Differential effects of oral versus intrathymic administration of polymorphic major histocompatibility complex class II Peptides on mononuclear and endothelial cell activation and cytokine expression during a delayed- type hypersensitivity response. Departament of pathology and Immunology, Monash Medical Schooll. Alfred Hospital, Prahran, Victoria, Australia. Am J Pathol 1994 Jun; 144 (6):1149- 58.
- Miller CC, Cook ME. Evidence against the induction of immunological tolerance by feeding antigens to chickens. Departament of poultry Science, University of wisconsin- Madison 53706. Poult Sci 1994 Jan; 73 (1): 106-12.
- Husby S, Mestcky J, Moldoveanu Z, Holland S, Elson CO. Oral tolerance in humans. T Cell but not B cell tolerance after antigen feeding. Departament of medicine. University of Alabama at Birmingham 35294. J Immunol 1994 May 1; 152 (9): 4663- 70.
- Feliziani V, Marfisi RM, Parmiani S, rush immunotherapy with sublingual administration of grass allergen extract. Allergol Immunopathol (Madr) 1993;21;173-8.
- Van Hoogstraten IM, Von Blomberg BM, Boden D, Kraal G, Scheper RJ. Non-sensitizing epicutaneous skin test prevent subsequent induction of immunotolerance. Deapartament of pathology, Vrije Universiteit, Amsterdam, the Nestherdans. J Invest Dermacol 1994 Jan; 102 (1): 80.
- Van Wilsem EJ, Van Hoogstraten IM, Breve J, Scheper RJ, Kraal G. Dendritic cells of the oral mucosa and the induction of oral tolerance. A local affair. Departament of cell Biology & Immunology, Vrije Universiteit, Amsterdam, The Netherlands. Immunology 1994 Sep; 83(1): 128-32.
- Takahashi I, Nakagawa I, Kiyono H, McGree JR, Clements JD, Hamada S. Mucosal T cells induce systemic anergy for oral tolerance. Departament of oral Microbiology, Osaka University Faculty of Dentistry, Japan. Biochem Biophys Res Commun 1995 Jan 5; 206 (1): 414-20.
- Matsui M, Kuroda Y. (Gut mucosal immunity and oral tolerance).Departament of Internal Medicine, Saga Medical School. Nippon-Rinsho 1994 Nov; 52 (11): 2873-9.
- Weiner L. Oral tolerance (comment). Center for Neurologic Diseases, Brighm and Women`s Hospital, Boston,MA 02115. Proc Natl Acad Sci U S A 1994 Nov 8; 91 (23): 10762-5.
- Yang R, Liu Q, Grosfeld JL, Pescovitz MD. Intestinal venous drainage through the liver is a prerequisite for oral tolerance induction. Departament of Surgery, Indiana University School of Medicine, Indianapolis. J Pedriatr Surg 1994 Aug; 29(8): 1145-8.
- Vistica BP, Chanaud NP, Felix N, Caspi RR, Rizzo LV, Nussenblatt RB, Gery I. CD8 T-cell are not essential for the induction of “Low – dose” oral tolerance Laboratory of Immunology, National Eye Institute, NIH, Berthesda, Maryland 20892. Clin Immunol Immunopathol 1996 Feb; 78 (2): 196-202.
- Fujihashi K, McGree JR, Yamamoto M, Hiroi T, Kiyono H. Delta T cells in Role of gamma the regulation of mucosal IgA response – and oral tolerance. Departament of Oral Biology, University of Alabama at Birmingham, 35294, USA. Ann N Y Acad Sci 1996 Feb 13; 778: 55- 63.
- Fukaura H, Kent SC, Pietrusewiez MJ, Kroury SJ, Weiner HL, Hafler DA. Induction of circulating myelin basic protein and proteolipid protein – specific transforming growth factor-beta 1-secreting TH3 T cells by oral administration of myelin in multiple sclerosis patients. Center for Neurologic Diseases, Deapartament of Neurology, Bringm and women`s Hospital, Boston, Massachusetts, USA. J Clin Ivest 1996 Jul 1; 98 (1): 70-7.
- Ke Y, Kapp JA. Oral antigen inhibits priming of CD8+CTL,CD4+T cells, and antibody responses while activating CD8+suppressor T cells. Departament of Pathology, Emory University School of Medicine, Atlanta, GA 30322, USA. J Immunol 1996 Feb 1; 156(3): 916-21.
- D`Ambrosio FP, Ricciardi Puccinelli P, Musarra A. Rush sublingual immunotherapy in parietaria allergic patients. Policlinico Universitario di Messina, Scuola di specializzazione in Allergologia ed Inmunología Clínica, Milano, Italia.. Allergol Immunopathol Madr 1996 Jul-Aug; 24(4): 146-51.
- Montgomery PC, Skandera CA, O`Sullivan NL. Fenotypic profile of lymphocyte population isolated from rat major salivary glands. Departament of Immunology and Microbiology, Wayne State University School of Medicine, Detroit, Michigan 48201, USA. Oral Microbiol Immunol 1996 Aug; 11 (4): 248-53.
- Quirino T, Iemoli E, Siciliani E, Parmiani S, Milazzo F. Sublingual versus injective inmmunotherapy in grass pollen allergic patients: a double blind (double dummy) study (see comments). Comments in: Clin Exp Allergy 1996 Nov; 26 (11): 1228-31. Servizio di Allergologia Ospedale L. Sacco, Milan, Italy. Clin Exp Allergy. 1996 Nov; 26 (11); 1253-61. Ciencias Biologicas, UFMG, Belo Horizonte. Brasil. Immunology 1993 Jan 78 (1): 147-51. 42. Malling HJ. Sublingual immunotherapy (editorial. Comment on; Clin Exp Allergy 1996 Nov; 26 (11); 1253-61. Clin Exp Allergy 1996 Nov; 26 (11): 1228-31.
- Yoshida T, Hachimura S, Kaminogawa S. The oral administration of low-dose antigen induces activation followed by tolerization, while high-dose antigenm induces tolerance without activation. Departament of Applied Biological Chemistry, University of Tokyo, Japan. Clin Immunol Immunopathol 1997 Mar; 82 (3): 201-15.
- Melamed D, Fishman Lovell J, Uni Z, Weiner HL, Friedman A. Peripheral tolerance of Th2 lymphocytes induced by continuos feeding of ovalbumin. Departament of Animal Sciences, Hebrew University of Jerusalem, Rehovot Israel. Int Immunol 1996 May; 8(5): 717-24.
- Kaminogawa S. Food allergy, oral tolerance and immunomodulation-their molecular and cellular mechanisms. Departament of Applied Biological Chemistry, University of Tokyo, Japan. Biosci-Biotechnol Biochem 1996 Nov; 60(11): 1749-56.
- Van Alteren AG, Van der Cammen MJ, Biewenga J, Savelkoul HF, Kraal G. Ig Eand Mast cell response on intestinal allergen exposure: a murin model to study the onset of food allergy. Department of Cell Biology and Immunology, Vrije Universiteit Amsterdam,The Netherlands. J Allergy Clin Immunology 1997 Jan; 99( 1 Pt 1): 94-9.
- Inada S, Yoshino S, Haque MA, Ogata Y, Kohashi O. Clonal anergy is a potent mechanism of oral tolerance in the suppression of accute antigen-induced arthritis in rats by oral administration of the inducing antigen. Departament of Microbiology, Saga Medical School,Japant. Cell Immunol 1997 Jan 10; 175(1); 67-75.
- Gamboa-P; Jauregui-I; Urrutia-I; Gonzalez-G; Antepara-I. Contact sensitization to cloxacillin with oral tolerance to other beta-lactam antibiotics. Section de Alergia-Inmunología, Hospital de Basurto. Contact Dermatitis 1996 Jan; 34(1): 75-6.
- Harper HM, Cochrane L, Williams NA. The role of small intestinal antigen-presenting cell in the induction of T-cell reactivity to soluble protein antigens; association between aberrrant presentation in the lamina propria and oral tolerance. University of Bristol, Departament of pathology and microbiology, School of Medical Sciences, University Walk, UK.. Immunology 1996 Nov;89(3): 449-56.
- ensitization to trimethoprim-sulfamethoxazole in acquired immune deficiency syndrome. Division of Allergy/Clinical Immunology, Departament of Medicine, Medicine state University of New York, Health Sciences Center at Brooklyn,USA. Ann Allergy Astma Immunol 1996 Nov; 77(5): 394-400.
- Kalanadhabhatta V, Muppidi D, Sahni H, Robles A, Kramer M. Successful oral des
- Van Wilsem EJ, Van Hoogstraten IM, Breve J, Sheper RJ, Kraal G. Dendritic cell of the oral mucosa and the induction of oral tolerance. A local affair. Immunology 1994; 83:128-32.
- Hasseus B, Dahlgren U, Bergenholz G Jontell M. Antigen presenting capacity of Langerhams cell from rat oral epithelium. Oral pathol Med 1995: 24: 56-60.
- Manetti R, Parronchi P, Giudizi M G, et al. Natural Killer cell stimulatory factor interleukin 12 (IL- 12) induces T helper type 1 (Th1) –specific immune responses and inhibits the development of IL-4- producing TH cell. Exp Med 1993; 177: 1199- 1204.
- Macatinia SE, Hosken NA, Litton M, et al. Dendritic cells produce Il- 12 and direct the development of TH1 cell from naive CD4+T cell. J Immunol 1995; 154: 5071, 9.
- Bagnasco M, Mariani G, Passalacqua G, et al. Absorption and distribution kinetics of the major Parietaria Judaica, allergen administered by noninjectable routes to healthy human beings. J Allergy Clin Immunol 1997, 100: 122-9.
- Greenberg MA Kaufman CR, Gonzales GE. Late and immediate systemic allergic reactions to inhalant allergen immunotherapy. J Allergy Clin Immunol 1986; 77: 865-70.
- Giovane Al, Bardare M, Passalacqua G, et al. A three- year double- blind placebo- controlled study with specific oral immunotherapy to Dermatophagoides: evidence of safety and efficacy in Pediatric patients. Clin Exp Allergy 1994; 24: 53-9.
- Johansson SGO, Deuschl H, Zetterstrom O. Use of glutar- aldehyde- modified timothy grass pollen extract in nasal hiposensitisation treatment of hay fever. Int Arch Allergy Appl Immunol 1979; 60: 447-60.
- Andri L, Senna G, Andri G, et al. Local nasal immunotherapy for birch allergic rhinitis with extract in powder form. Clin Exp Allergy 1995; 25: 1092-9.
- Ariano R, Panzani RC, Chiapella M, Augeri G, Falagiani P. Local immunotherapy of seasonal allergic rhinitis in children due to Parietaria Pollen. A preliminary report. Pediatric Asthma Allergy Immunol 1993; 7: 227-37.
- Welsh PW, Butterfield JH, Yunginger W, Agarwal MK, Gjeich GJ. Allergen controlled study of intranasal immunotherapy for ragweed hay fever. J Allergy Clin Immunol 1983; 71: 454-60.
- Crimi E, Voltolini S, Troise C, et al. Local immunotherapy with Dermatophagoide extract in asthma. J Allergy Clin Immunol 1991; 87: 721-8.
- Tari MG, Mancino M, Monti G. Immunotherapy by inhalation of allergen in powder in house dust allergic asthma; a double – blind study. J Investing Allergol Clin Immunol 1992; 2: 59-67.
- Taurdorf E, Laursen LC, Djurup R, et al. Oral administration of grass pollen to hay fever patients. An efficacy study in oral hiposensitization. Allergy 1985; 40: 321-35
- Mosbech H, Dreborg S, Madsen F, et al. Night dose grass pollen tablets use for hyposensitization in hay fever patients. A one- year double blind placebo controlled study. Allergy 1987; 42: 451-5.
- Taudorf E, Laurse LC, Lanner A, et al. Oral immunotherapy in birch pollen hay fever. Allergy Clin Immunol 1987; 80: 153-61.
- Scadding K, Brostoff J. Low dose sublingual therapy in patients with allergic rhinitis due to dust mite. Clin Allergy. 1986; 83, 589, 94.
- Nelson HS, Oppenheimer J, Vatsia GA, Bucheimer A.A double blind placebo controlled evaluation of sublingual immunotherapy with standardized eat extract. J Allergy Clin Immunol 1993; 92: 229-36.
- Casanova M, Guerra F, Moreno C, Miguel R, Maranon F, Daza JC. Double blind placebo controlled – clinical trial of preseasonal treatment with allergic extracts of Olea europea pollen administered sublingually. J Investing Allergol Clin Immunol 1994; 4: 305-14.
- Tari MG, Mancino M, Monti G. Efficacy of sublingual immunotherapy in patients with rhinitis and asthma due to house dust mite. A double blind study. Allergol Immunopathol Madr 1990; 18: 277- 84.
- Sabbah A, Hassoun S, Le Scllin J, André C, Sicard H. A double blind placebo controlled trial by the sublingual route of immunotherapy with a standardized grass pollen extract. Allergy 1994; 49: 309-13.
- Troise C, Voltolini S, Canessa A, Pecora S, Negrini AC. Sunblingual immunotherapy in parietaria pollen induced rhinitis; a double blind study. J Investig Allergol Clin Immunol 1995; 5: 25-30.
- Hirsch T Sahn M, Leupoid W. Double- blind placebo- controlled study of Sunblingual immunotherapy with house dust mite extract (D, pt.) in Children.Pediatric Allergy immunol 1997; 8: 21-7.
- Passalacqua G, Albano M, Fregonese L, et al. Randomised controlled trial of local allergoid immunotherapy on allergie inflammation in mite- induced rhinoconjuntivitis. Lancet. 1998; 351, 629, 32.
- Watkin AD. The role of alternative therapies in the treatment of allergic diseases. Clin Exp Allergy 1994; 24: 813-25.
- Malling HJ, Abreu- Nogueira J, Alvarez, Cuesta E, Bjorkstén B, Bousquet J, Cailot D, Canonica GW, Passalacqua G, Saxonis- apageorgiou P, Valovirta E. Local immunotherapy. Allergy 1998; 53: 933-944.
- Howard L.Weiner, E.P.Rees. Mucosal tolerance. Immunology Letters. 1999; 69:1.
- A.M.C Faria.Weiner. Oral tolerance mechanisms and therapeutics
- applications, Adv. Immunol 1999; 73: 153-264. E,Williamson Viney J. Joanne L, Viney. Department of Molecular Immunology Immunex Corporation email: williame@immunex.com o jviney@immunex.com. Dendrictic Cell are Key Regulators of Intestinal Immune Response. Mucosal Immunology Update 1999; (7), 2: 7.
- Brandizaeg P. History of oral tolerance and mucosal immunity. Laboratory for Immunohistochemistry and Immunopathology. Institute of Pathology, University of Oslo, Norway. Ann N Y Acad Sci 1996; Feb 13; 778: 1-27.
- Hafler DA, Weiner HL. Antigen-specific immunosuppression: Oral tolerance for the treatment of autoimmune diseases. Laboratory of Molecular Immunology, Center for Neurologic Diseases, Brigham and Women´s Hospital, Bosten, Mass. Chem Immunol1995; 60: 128-49.
- Palacios AS, Medina FS, Rua-Figueroa Al, Millares CB, Santos SR, Marrero JAG, Comparative clinical-immunological study of oral and subcutaneous immunotherapy in children with extrinsic bronchial astma. Allergol Immunopathol Madr 1989;17:323-9.
- Marth T, Strober W, Kelsall BL. High dose oral tolerance in ovalbumin TCR-trangenic mice; systemic neutralization of IL-12 augments TGF-b secretion and T cell apoptosis. Laboratory of Clinical Investigation, National Institute of Allergy and Infectious Diseases, Bethesda, MD 20892, USA. J Immunol 1996 Sep 15; 157 (6): 2348-57.
- Kelly KA, Whitacre CC. Oral tolerance in EAE; reversal of tolerance by T helper cell cytokines. Departament of Microbiology and Immunology, University of Arkansas for Medical Sciences, Little Rock 72205, USA. J Neuroimmunol 1996 May; 66(1-2): 77-84.
- Holt PG, Britten D, Sedgewick JD. Suppression of IgE responses by antigen inhalation: Studies on the role of genetic and environmetal factors. Immunology 1987, 60: 97-102.
- Wang ZY, Link H, Ljungdahl A, et al. Induction of g interferon-, interleukin- 4, and transforming growth factor-b1 in rats orally tolerized against experimental autoimmune myasthenia gravis. Departament of Neurology, Karolinska Institute, Huddinge University Hospital, Stockolm, Sweden. Cell Immunol 1994 Sep; 157 (2): 353- 68.
- Wang ZY, Link H, Ljungdahl A, et al. Induction of g interferon-, interleukin- 4, and transforming growth factor-b1 in rats orally tolerized against experimental autoimmune myasthenia gravis. Departament of Neurology, Karolinska Institute, Huddinge University Hospital, Stockolm, Sweden. Cell Immunol 1994 Sep; 157 (2): 353- 68.
- Zettel L, Clark DA, Ernst PB. Transforming growth factor-b1 enhances Ig.G and Ig.A sheep red blood cell responses. Molecular Virology and Immunology program, McMaster University, Hamilton, Ontario, Canadá. Int Immulol 1992 sept; 4-(9): 975-83.