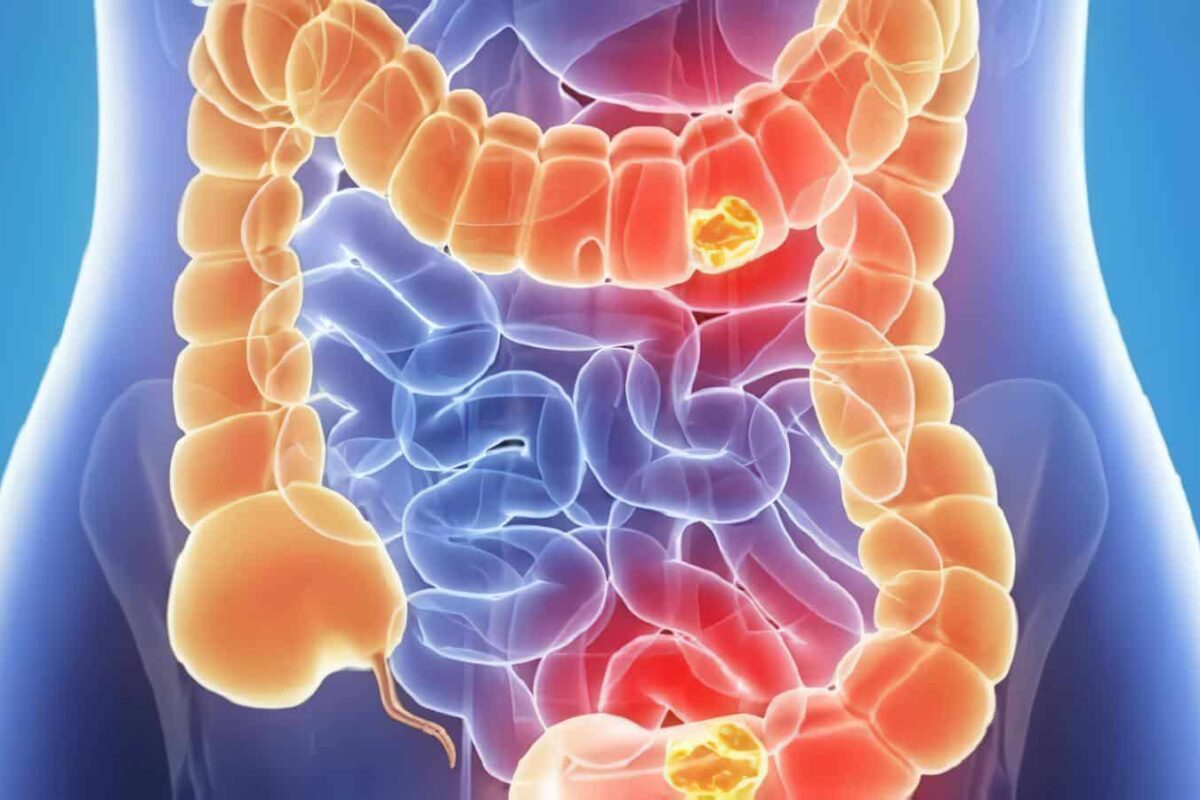
Los pacientes con colitis ulcerativa tienen un riesgo más alto de padecer cáncer colorrectal que la población general. Este riesgo es relacionado con la extensión y duración de la enfermedad, pero no con su actividad.
A continuación se describen las estrategias de vigilancia para evitar el cáncer colorrectal. Recordemos que éstos no son más que normas generales que deben ser interpretadas en forma individual en cada paciente.
Indicaciones de vigilancia para cáncer colorrectal en colitis ulcerativa
- Colitis ulcerativa por 8 o más años.
- Colitis ulcerativa del lado izquierdo por 15 años o más.
- Proctitis: screening y seguimiento de acuerdo a los parámetros de la población general.
- Colangitis esclerosante primaria; comenzar vigilancia en el momento del diagnóstico.
Técnica. Se realiza una colonoscopia hasta el ciego tomando al menos 33 biopsias jumbo o biopsias en 4 cuadrantes cada 10 cms.
Hallazgos y conducta a seguir.
- Sin displasia. Repetir vigilancia en 1 ó 2 años.
- Indefinido para displasia. Se trata la inflamación activa y se repite vigilancia en 6 meses.
- Displasia plana. Aquí es importante confirmarla por un segundo patólogo, hay controversia cuando se trata de una displasia de bajo grado debido a la dificultad para distinguir entre atipia reactiva y ésta. Algunos pacientes desean seguir sometidos a vigilancia y se recomienda en este caso seguirlos a 6 meses. Otro grupo es partidario de realizar colectomía. Cuando se trata de una displasia de alto grado se recomienda colectomía definitivamente.
- Lesión displásica o masa. Cuando se trata de una lesión o masa asociada con displasia (LMAD) se recomienda colectomía. Si se encuentra un adenoma característico se procederá a la polipectomía; si en el estudio histológico se encuentra displasia en la mucosa adyacente se indica la colectomía. Y si no hay displasia en la mucosa adyacente el paciente se someterá a vigilancia a un año (77, 82,83).
Prevención del cáncer en la EC
Mucho menor es la atención dedicada a reducir el riesgo de un cáncer colorrectal en los pacientes con EC. Muchos de ellos han sido sometidos a resecciones de la parte afectada del colon, con lo que el riesgo quedaba reducido.
Dada la naturaleza irregular de la EC, una colectomía total raras veces estará justificada en ausencia de una afectación cólica total. Se recomienda la inclusión de los pacientes con una colitis de Crohn de larga duración en los programas de vigilancia del cáncer aunque se reconoce que se disponen de pocos datos en apoyo a esta recomendación (82).
Referencias
- 1. Fiocchi C. Inflammatory Bowel Disease. Etiology and Pathogenesis. Gastroenterology 1998; 115: 182-203.
2. Asher K, Sachar D. Treatment. Guide Line: Ulcerative Colitis Practice guide line in Adults. Am J Gastroenterol 1997; 4: 137-141. - 3. Gonzalez V, Perez J, Carneros J. Advances in Chronic Intestinal Inflammatory Disease. Gastroenterologia Integrada 2000; 1: 155-170.
- 4. Pietro G, Friedman L. Epidemiología y Evolución Natural de la Enfermedad Inflamatoria Intestinal.Clínicas de Gastroenterología de Norte América 1999:275-308.
- 5. Lapidus A, Bernell O, Hellers G. et al. Incidence of Crohn’s Disease in Stockholm county. 1955-1.989. Gut 1.997; 41: 480-486.
- 6. Stowe S, Redmond. S, Stormont J, et al. An Epidemiologic Study of Inflammatory Bowel Disease in Rochester, New York. Gastroenterology 1990; 98: 104-110.
- 7. Devlin H, Datta D, Dellipiani A. The incidence and prevalence of Inflammatory Bowel Disease in North Tees. Health; District. World J Surg 1980. 4: 183-193.
- 8. Roth M, Petersen G, McElree C. et al. Geographic origins of jewish patients with. inflammatory Bowel Disease. Gastroenterology 1989; 97: 900-904.
- 9. Kurata J, Kanto S, Frankl H, et al. Crohn´s Disease among ethnic groups in 4 large health mantenance organizations. Gastroenterology 1992; 102: 1940-1948.
- 10. Calkins BA. Meta-Analysis of the role of smoking in Inflammatory Bowel Disease. Dig Dis SCI 1989; 34: 1841-1854.
- 11. Tobin M, Lugan R, Langman M, et al. cigarrette smoking and Inflammatory Bowel Disease. Gastroenterology 1987; 93: 316-321.
- 12. Vessey M, Jewell D, Smith A, et al. Chronic Inflammatory Bowel Disease, cigarrette. smoking and use of oral contraceptives findings in a large cohort study of women of childbearinsgage. Br Med J 1986; 29: 1101-1103.
- 13. Timmer A, Sutherland L, Martin F, et al. Oral contraceptive use and smoking are risk factors for relapse in Crohn’s disease. Gastroenterology 1998; 114: 1143-1150.
- 14. Russel M, Volovics A, Schoon J, et al. Inflammatory bowel disease is there any relation between smoking status and this is presentation? IBD 1998; 4: 182-186.
- 15. Cosnes I, Carbonnel F, Carrat F. et al. Effects of current and former cigarrette smoking on the clinical course of Crohn’s disease. Pharmacol Ther 1994; 13: 1403-1411.
- 16. Cosnes J, Carbonnel F, Carrat F, et al. Oral contraceptive use and the clinical course of Crohn’s disease: A prospective cohort study. Gut 1999;45: 218-222.
- 17. Mahadevan U, Loftus E, Tremaine W, et al. Safety of selective Cyclooxygenase-2 inhibitors in Inflammatory Bowel Disease. 2002; 97: 910-914.
- 18. Jarnerot G, Jarnmar I, Nilssun K. Consumption of refined sugar by patients with Crohn’s Disease Ulcerative Colitis, or irritable Bowel. Scand J Gastroenterol 1983; 18: 999-1002.
- 19. Reif S, Klein I, Lubin M. Antecedentes dietarios en la Enfermedad Inflamatoria Intestinal. Gut 1997; 40: 754-760.
20. Jones P, Fine P. Crohn’s Disease and Measles. Lancet 1997; 344: 473. - 21. Finney M, Clegg A, Winwood P, et al. A study of case control in vaccination of Inflammatory bowel disease. Lancet 1997; 350: 764-766.
- 22. Fischer N, Yee L, Nightingale P. Measles virus serology in Crohn’s disease. Gut 1997; 41: 66-69.
- 23. Campieri M, Giunchetti P. Bacteria as the cause of ulcerative colitis. Gut 2001;48: 132-135.
- 24. Lisby G, Andersen J, Eng Baerk, et al . Mycobacterium paratuberculosis in intestinal tissue from patient with Crohn’s Disease demonstrated by nested polymerase. Chain Reaction Scand. J Gastroenterol 1994; 29: 923-929.
- 25. Colombel J, Cortot A, Vankruining H. Therapy Update Antibiotic in Crohn’s . Gut 2001; 48: 647-649.
- 26. Russel M, Durante, Brummer J, et al. Appendectomy an the risk of developing ulcerative colitis or Crohn’s disease: results of a large case – control study South Limburg inflammatory bowel disease study group. Gastroenterology 1997; 113: 377-382.
- 27. Yang H, Mc Elree C, Ruth, et al. Familiar empirical, risk for Inflammatory Bowel Disease: differences between Jews and Non – Jews. Gut 1997; 34: 517-524.
- 28. Satsangi J, Grootschulten C, Holt H, et al. Clinical Patterns of Familiar Inflammatory Bowel Disease. Gut 1997; 40: 572-574.
- 29. Watts D, Satsangi J. The Genetic Jigssaw of Inflammatory Bowel Disease. Gut 2002; 50: 31-36.
- 30. Sandbor W, Landers C, Tremaine W, et al. Antineutrophil cytoplasmic antibody, correlates with chronic pouchitis after ileal pouch – anal anastomosis. Am J Gastroenterol 1995; 90: 740-742.
- 31. Satsangi J, Landers C, Koos K, et al. The presence of anti-neutrophil antibodies reflects clinical and genetic heterogeneity within inflammatory bowel disease. Inflamm Bowel Disease. Inamm Bowel Dis 1998; 9: 18-26.
- 32. Isolauri P, Kir Javainen S. Salminen probiotic A rule in the treatment of Intestinal Infection and Inflammation. Gut 2002; 50: 54-59.
- 33. Archila P, Montoya A. Intestino Grueso. Enfermedad Inflamatoria Intestinal. En: Hani A, Gutiérrez O, Alvarado J, eds, Gastroenterología. Bogotá: Editorial McGraw-Hill; 2001: 171-177.
- 34. Hamilton S, Morsun B. Crohn’s disease. In: Haubrich W, Schaffner F, Berk J, eds, Gastroenterology. Bockus Philadelphia: Editorial WB. Saunders company; 1994: 1398-1438.
- 35. Farmer R. Ulcerative Colitis. In: Haubrich W, Schaffner F, Berik J. eds. Gastroenterology. Bockus Philadelphia: Editorial W.B Saunders company; 1994: 1326-1352.
- 36. Costell D. American college of Physicans. Intestino Grueso. Enfermedades Inflamatorias del intestino. MKSAP. Programa de actualización en Gastroenterologia y Hepatología, 2a ed. Educación médica continua. Bogotá; 1999: 95-102.
- 37. Hanauer S, Sandborn W. Management of Crohn’s Disease in Adults. Am J Gastroenterol 2001; 96: 635-643.
- 38. Sutherland L, Roth, Beck P, et al. Oral 5-AAS for inducing remission in ulcerative colitis in the Cochrane library. Issue 2, 2001. Oxford Update Software.
- 39. Campieri M. New steroids and new salicylates in Inflammatory Bowel Disease. A critical appraisal. Gut 2002; 50: 43-46.
- 40. Marteau P, Crand J, Focault M. Use of mesalazine slow release suppositories 1 gr three times per week to maintain remission of ulcerative proctitis a randomized double blind placebo controlled multicentre study. Gut 1998; 42: 195-199 .
- 41. D´Albasia G, Parini E, Camarry E, et al. Combined terapy with 5-AAS. Tablets and enemas for mataining remission in ulcerative colitis a randomized double blind study. Am J Gastroenterol 1997;92: 1143-1147.
- 42. Caprilli R, Andreuli A, Caparsu L, et al. Oral mesalazine for the prevention of postoperative recurrence of Crohn’s Disease. Grupo Italiano
- per la studie del colon e del retto (gisc). Aliment Pharmacol Ther 1994; 8: 35-43.
- 43. Mc Leod R, Wulffb, Stein A, et at. Prophylact
- 44. Brignola C, Cottone M, Pere A, et al. Mesalazine in the prevention of endoscopic recurrence, after intestinal resection for Crohn´s Disease. Gastroenterology 1995; 108: 345-349.
- 45. Lochsh H, Mayer M, Fleigh W, et al. Prophylaxis of postoperative relapse in Crohn´s Disease with mesalazine. European Cooperative Crohn’s Disease Study VI. Gastroenterology 2000; 118: 246-273.
- 46. Summer R, Switz D, Session J. et al. National Cooperative Crohn’s Disease study. Gastroenterology 1999; 77: 847-869.
- 47. Malchow H, Ewe K, Brand’s J, et al. European Cooperative Crohn’s Disease study. Gastroenterology 1984; 86: 244-266.
- 48. Modigliani G, Mary J, Simon J, et al. Clinical, biological and endoscopy picture of attacks of Crohn’s Disease evolution on prednisolone. Gastroenterology 1990; 98: 811-818.
- 49. Campieri M, Ferguson A. DaeW, et al. Oral budesonide with prednisolone for active Crohn’s Disease. Gut 1997: 209-214.
- 50. Sachar D. Maintenance therapy in ulcerative colitis an Crohn’s disease. J Clin Gastroenterol 1994; 20: 117-122.
51. Cortot A, Colombel F, Rutgeerts P, et al. Swift from systemic steroid dependent patients with inactive Crohn’s Disease. Gut 2001; 48: 186-198. - 52. Gomollon F, Hinojosa J, Nos P. Budesonide and Inflamamatory Bowel Disease.Gastroenterol Hepatol 1999;22: 525-532.
- 53. Fraser A. G, Orchard T, Jewell D. The efficacy of azathioprine for the freatment of Inflammatory Bowel Disease A 30 year review. Gut 2002; 50: 485-489.
- 54. Sandbor W. Azathioprine: state of the art in Inflammatory Bowel Disease. Scand J Gastroenterol 1998; 225: 92-99.
55. Egan L, Sanburn W. Methrotexate for Inflammatory Bowel Disease. Pharmacology and preliminary results. Mayo Clin Proc 1996; 71: 69-80. - 56. Feagan B, Rochin J, Fedorak R, et al. Methrotexate for the treatment of Crohn’s Disease. N Engl J Med 1995; 332: 292-297.
- 57. Feagan B, Fedorak R, Irvine E. A comparison of Methrotexate with placebo for the maintenance of remision in Crohn´s Disease. N Engl J Med 2000; 1627-1632.
- 58. Ramptun DS. Therapy Update Methrotexate in Crohn´s Disease. Gut 2001; 48: 790-791.
- 59. Stein R, Hanauer S. Medical therapy for Inflammatory Bowel Disease. Clin-North AM 1994: 297-321.
- 60. Lichtiger S, Present D, Korn-Blutha, et al. Cyclosporin in severe ulcerative colitis refractary to steroid therapy. N Engl J Med 1994; 330: 1841-1845.
- 61. Lichtenstein G. Special reports and reviews treatment of fistulizang Crohn´s Disease. Gastroenterology 2000; 119: 1132-1147.
- 62. Sand B. Nuevas formas de tratamiento de la enfermedad inflamatoria Intestinal. Clínicas de Gastroenterología de Norte América 1999; 2: 357-391.
- 63. Hinojosa J. Anti-tumor necrosis factor antibodies in the treatment of Inflammatory Bowel Disease. Gastroenterol Hepatol 2000; 23: 250-257.
- 64. Konstantines A, Papadakis A ,Targan S. Tumor necrosis factor biology and therapeutic inhibitors. Gastroenterology 2000; 119: 1148-1157.
- 65. Hanauer S, Feagan B, Lichtenstein G, et al. Maintenance infliximab for Crohn´s Disease the ACCENT I randomised trial. Lancet 2002; 359: 1541-1549.
- 66. Rutgeerts P, D´Haens G, Targan S, et al. Efficacy and safety of retreatment with anti-tumor necrosis factor antibody (infliximab) to maintain remission in Crohn’s disease. Gastroenterology 1999; 117: 761-769.
- 67. O´Sullivan M, Omorain C. Therapy Update. Liquid diets for Crohn´s Disease. Gut 2001: 48: 757-758.
- 68. Segain. JP, De la Bletiere DR, Bourreille A, et al. Butyrate inhibit Inflammatory. Responses through NFkB inhibition implication for Crohn’Disease. Gut 2000; 47 : 397-403.
- 69. Luhrs H, Gerke T, Muller J, et al. Butyrate inhibits NF-KAPPA B activation in lamina propia macrophagues of patients with ulcerative colitis. Scand J Gastroenterol 2002; 37: 458-466.
- 70. Colombee J, Cortot A, Kruiningen H. Therapy Update. Antibiotics in Crohn´s Disease. Gut 2001; 48: 647-649.
- 71. Feagan B, Fedorak R, Irving J. A comparision of Methrotexate with placebo for the maintenance of remission in Crohn´s disease. 2000; 342: 1627-1632.
- 72. Turumen U, Farkkila M, Hakala K, et al. Long-term treatment of ulcerative colitis with cyprofloxacine: a prospective, double-blind, placebo controlled study. Gastroenterology 1998; 115: 1072-1078.
- 73. Gionchetti, Rizzelo F, Ferrieri A, et al. Rifaximin in patients with moderate or severe ulcerative colitis refractory to steroid treatment: a double-blind, placebo – controlled trial. Dig Dis Sci 1999; 44: 1220-1221.
- 74. Isolauri E, Kirjavainen P, Salminen S. Probiotic a rule in the treatment of intestinal. infection and inflammation? Gut 2002; 50: 54-59.
- 75. Rembacken B, Snelling A, Hawikey P, et al. Now-Pathogenic. Escherichila coli versus mesalazine for the treatment of ulcerativ ecolitis a randomised trial. Lancet 1999; 354: 635-639.
- 76. Gionchetti P, Rizzello F, Ventuari A, et al. Oral bacteriotherapy as maintenance treatment in patients with chronic pouchitis: a double blind placebo-controlled trial. Gastroenterology 2000; 119: 305-309.
- 77. Farell R, Peppercorn M. Seminar ulcerative colitis. Lancet 2002; 359: 331-340.
- 78. Guslandi M, Tittobello A. Outcome of ulcerative after treatment with trasdermal nicotine. Eur J Gastroenterol Hepatol 1998; 10: 513-515.
- 79. Van Deventer. Small therapeutic molecules for the treatment of inflammatory bowel disease. Gut 2002; 50: 47-53.
- 80. Panes J. Adhesion molecules: their rule in the physiopathology and treatment of inflammatory bowel disease. Gastroenterol Hepatol 1999; 22: 514-524.
- 81. Yacyshyn B, Chey W, Guff J, et al. Double blind placebo controlled trial of the remission inducing and steroid sparing properties of an ICAM-1. antissense. Oligodeo-xyneuclotide, alicarfosen (ISIS 2302), inactive steroid dependent Crohn´s Disease. Gut 2003; 51: 30-36.
- 82. Becker J. Tratamiento quirúrgico de la colitis ulcerosa y la enfermedad de Crohn. Clínicas de Gastroenterología de Norte América 1999; 2: 415-439.
- 83. Rubin P, Friedmans S, Harpaz N, et al. Colonoscopic polypectomy in chronic colitis. Conservative management after endoscope resection of dysplactic polyps. Gastroenterology 1999; 117: 1295-1300.