Estudios recientes del registro internacional muestran una disminución en el uso del soporte de vida extracorpórea neonatal, presumiblemente por la efectividad de los tratamientos descritos previamente como el ONI y la administración exógena de surfactante en infantes cercanos al término.
Sin embargo, no todos los infantes responderán a estos nuevos tratamientos.
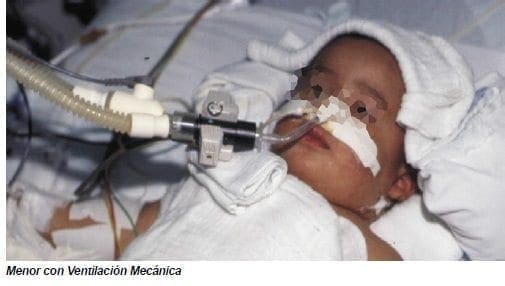
La oxigenación de membrana extracorpórea se usa para tratar la falla respiratoria aguda cuando otras modalidades de tratamiento han fallado. El ECMO había demostrado que mejoraba la sobrevida en infantes a término y cercanos al término con falla respiratoria severa en al menos dos estudios clínicos controlados de instituciones individuales.
En forma subsecuente, el estudio aleatorizado colaborativo del Reino Unido de ECMO Neonatal y los estudios de seguimiento muestran que el ECMO en forma significativa reduce el riesgo de muerte sin aumentar el de secuelas severas. En este estudio, 30 de 93 infantes en el grupo de ECMO murieron comparado con 54 de 92 en el grupo de cuidado convencional.
Los infantes con hernia diafragmática, no son propensos a responder al óxido nítrico y tienen más pobre desenlace que otros pacientes que reciben oxigenación de membrana extracorpórea con una sobrevida del 62% comparado con 83% en infantes sin hernia diafragmática.
Sin embargo, sin ECMO, infantes con hernia diafragmática que desarrollan hipoxemia refractaria tienen una alta mortalidad.
En un reciente estudio británico, ninguno de los 17 infantes con HDC enrolados y aleatorizados al grupo control sobrevivieron mientras que 4 de 18 infantes que recibieron ECMO sobrevivieron. El ECMO venovenoso, que es usado menos frecuentemente, es preferible al ECMO venoarterial en la falla respiratoria aguda, puesto que evita la canulación de la arteria carótida y parece tener menores complicaciones.
Nuevas técnicas de intercambio gaseoso extracorpóreo, como el método de la cánula de luz única de empuje y halado, conocido como AREC (asistencia respiratoria extracorpórea), provee soporte efectivo en neonatos y es más rápido de aplicar puesto que la canulación es generalmente percutánea y más fácil de operar.
La consideración de la terapia con ECMO debe incluir una evaluación de los riesgos versus los beneficios por la naturaleza invasiva de la terapia y la necesidad de heparinización. Los criterios usuales para el soporte con ECMO incluyen:
- Más de 34 semanas de gestación.
- Peso mayor de 2000 grs.
- Ecografía transfontanelar sin hemorragia intracraneana mayor.
- Enfermedad pulmonar reversible y soporte con ventilación mecánica durante no más de 14 días.
- Sin evidencia de anomalías congénitas letales.
El momento de referencia al centro de ECMO es crítico.
Tan reciente como hace 15 años la mortalidad por la FHRN era del 40% con una incidencia de secuelas neurológicas mayores del 15-60%.
Si todas las terapias de rescate disponibles incluyendo el ECMO se utilizan, la mortalidad es actualmente menor del 20-25% y la incidencia de secuelas neurológicas mayores para los infantes sobrevivientes es aproximadamente del 15-20%.
La referencia y transporte al centro de ECMO neonatal debe realizarse antes de hipoxemia refractaria.
La consulta temprana y la discusión con el centro de ECMO se recomienda fuertemente.
Guías para consulta están publicadas en la página web de la organización de soporte de vida extracorpórea (http://www.elso.med.umich.edu/).
Referencias Bibliográficas
- 1. Abman SH, Griebel JL, Parker DK, Schmidt JM, Swanton D, Kinsella JP. Acute effects of inhaled nitric oxide in severe hypoxemic respiratory failure in pediatrics. J Pediatr 1994;124:881-8.
- 2. Abman SH: New developments in the pathogenesis and treatment of neonatal pulmonary hypertension. Pediatr Pulmonol Suppl 1999; 18: 201-4.
- 3. Alano MA, Ngougmna E, Ostrea EM Jr, et al: Analysis of nonsteroidal antiinflammatory drugs in meconium and its relation to persistent pulmonary hypertension of the newborn. Pediatrics 2001 Mar; 107(3): 519-23.
- 4. Al-Mateen KB, Dailey K, Grimes MM, Gutcher GR. Improved oxygenation with exogenous surfactant administration in experimental meconium aspiration syndrome. Pediatr Pulmonol 1994;17:75-80.
- 5. Auten RL, Notter RH, Kendig JW, et al: Surfactant treatment of full-term newborns with respiratory failure. Pediatrics 1991 Jan; 87(1): 101-7.
- 6. Auten RL, Vozzelli M, Clark RH. Volutrauma. What is it, and how do we avoid it? Clinics in Perinatology 2001. 28(3):505-15.
- 7. Beckman JS, Beckman TW, Chen J, Marshall PA, Freeman BA. Apparent hydroxy radical production by peroxynitrite: implications for endothelial injury from nitric oxide and superoxide. Proc Natl Acad Sci USA 1990; 87:1620-4.
- 8. Blanke JG, Jorch G:. Surfactant therapy in severe neonatal respiratory failure – multi-center study – II. Surfactant therapy in 10 newborn infants with meconium aspiration syndrome. Klinische Padiatrie 1993;205(2):75-78.
- 9. Braner DA, Fineman JR, Change R, Soifer SJ. M&B 22948, a cGMP phosphodiesterase inhibitor, is a pulmonary vasodilator in lambs. Am J Physiol 1993; 264:H252-H258.
- 10. Brower RG, Ware LB, Berthiaume Y, Matthay, MA. Treatment of ARDS. Chest 2001;120(4):1347-1367.
11. Brown DL, Pattishall EN. Other uses of surfactant. Clin Perinatol 1993;20:761-89. - 12. Chen CT , Toung TJK, Rogers MC. Effect of intra-alveolar meconium on pulmonary surface tension properties. Crit Care Med 1985;13:233-236.
- 13. Cochrane CG, Revak SD, Merritt TA, et al. Bronchoalveolar Lavage with KL4-Surfactant in Models of Meconium Aspiration Syndrome. Pediatric Research. 1998. 44(5):705-715.
- 14. Clark DA, Nieman GF, Thompson JE, et al. Surfactant displacement by meconium free fatty acids: An alternative explanation for atelectasis in meconium aspiration syndrome. J Pediatr 1987;110:765.
- 15. Clark RH, Yoder BA, Sell MS. Prospective, randomized comparison of high-frequency oscillation and conventional ventilation in candidates for extracorporeal membrane oxygenation. Journal of Pediatr 1994; 124(3):447-54.
- 16. Clark RH, Gerstmann DR: Controversies in high-frequency ventilation. Clin Perinatol 1998 Mar; 25(1): 113-22.
- 17. Clark RH, Kueser TJ, Walker MW, et al. Low-dose nitric oxide therapy for persistent pulmonary hypertension of the newborn. Clinical Inhaled Nitric Oxide Research Group. N Engl J Med 2000 Feb 17; 342(7): 469-74.
- 18. Clark RH, Gerstmann DR, Jobe AH, et al. Lung injury in neonates: Causes, strategies for prevention, and long-term consequences. Journal of Pediatr 2001;139(4):478-484.
- 19. Collet-Martin S, Gatecel C, Kermarrec N, et al. Alveolar neutrophil functions and cytokine levels in patients with the adult respiratory distress syndrome during nitric oxide inhalation. Am J Respir Crit Care Med 1996;153:985-90.
- 20. Cornish JD, Heiss KF, Clark RH, Strieper MJ, Boecker B, Kesser K. Efficacy of venovenous extracorporeal membrane oxygenation for neonates with respiratory and circulatory compromise. J Pediatr 1993;122:105-9.
- 21. Davey AM, Becker JD, Davis JM. Meconium aspiration syndrome: physiological and inflammatory changes in a newborn piglet model. Pediatr Pulmonol 1993;16:101-8.
- 22. Davidson D, Barefield ES, Kattwinkel J, et al. Inhaled nitric oxide for the early treatment of persistent pulmonary hypertension of the term newborn: a randomized, double-masked, placebo-controlled, dose-response, multicenter study. The I-NO/PPHN Study Group. Pediatrics 1998;101:325-34.
- 23. Davidson D, Barefield ES, Kattwinkel J, et al. Safety of withdrawing inhaled nitric oxide therapy in persistent pulmonary hypertension. Pediatrics 1999;104:231-6.
- 24. Delius R, Anderson H, Schumacher R, et al. Venovenous compares favorably with venoarterial access for extracorporeal membrane oxygenation in neonatal respiratory failure. J Thorac Cardiovasc Surg 1993;106:329-38.
- 25. Diniz EMA, Fiori RM:. Curosurf therapy in severe meconium aspiration (MAS). Biol Neonate 1995;67 (Suppl):86.
- 26. Driscoll W, Thurin S, Carrion V, et al. Effect of methylene blue on refractory neonatal hypotension. J Pediatr 1996;129(6):904-908.
- 27. Drummond WH, Gregory G, Heymann MA, Phibbs RA. The independent effects of hyperventilation, tolazoline, and dopamine on infants with persistent pulmonary hypertension. J Pediatr 1981; 98:603-11.
- 28. Durandy Y, Chevalier JY. Single-cannula venovenous bypass for respiratory membrane lung support. J Thorac Cardiovasc Surg 1990;99:404-9.
- 29. Ekekezie II, Thibeault DW, Garola RE, Truog WE. Monocyte Chemoattractant Protein-1 and Its Receptor CCR-2 in Piglet Lungs Exposed to Inhaled Nitric Oxide and Hyperoxia. Pediatr Res 2001:50(5):633-640.
- 30. Fauza DO, Hirschl RB, Wilson JM. Continuous intrapulmonary distension with perfluorocarbon accelerates lung growth in infants with congenital diaphragmatic hernia: initial experience. J Pediatr Surg 2001;36(8):1237-40.
- 31. Findlay RD, Taeusch HW, Walther FJ: Surfactant replacement therapy for meconium aspiration syndrome. Pediatrics 1996 Jan; 97(1): 48-52.
- 32. Fineman JR, Soifer SJ, Heymann MA: Regulation of pulmonary vascular tone in the perinatal period. Ann Rev Physiol 1995; 57: 115-34.
- 33. Finer NN, Etches PC, Kamstra B, Tierney AJ, Peliowski A, Ryan CA. Inhaled nitric oxide in infants referred for extracorporeal membrane oxygenation: dose response. J Pediatr 1994;124:302-8.
- 34. Finer NN, Barrington KJ: Nitric oxide for respiratory failure in infants born at or near term (Cochrane Review). Cochrane Database Syst Rev 2000;2: CD000399.
- 35. Finer NN, Sun JW, Rich W, et al. Randomized, prospective study of low-dose versus high-dose inhaled nitric oxide in the neonate with hypoxic respiratory failure. Pediatrics 2001;108(4):949-55.
- 36. Fox WW, Greenspan JS, Hirschl RL, et al. Alveolar Recruitment During and After Tracheal Instillation of LiquiVent (R) in Infants on Partial Liquid Ventilation (PLV). Pediatr Res 1997;41(4) Part 2:253.3
- 7. Gerlach H, Rossaint R, Pappert D, Falke KJ. Time-course and dose-response of nitric oxide inhalation for systemic oxygenation and pulmonary hypertension in patients with adult respiratory distress syndrome. Eur J Clin Invest 1993;23:499-502.
- 38. Gersony WM. Neonatal pulmonary hypertension: pathophysiology, classification and etiology. Clin Perinatol 1984;11:517-24.
- 39. Goldman AP, Tasker RC, Haworth SG, Sigston PE, Macrae DJ. Four patterns of response to inhaled nitric oxide for persistent pulmonary hypertension of the newborn. Pediatrics 1996;98:706-13.
- 40. Halliday HL, Speer CP, Robertson B, et al: Treatment of severe meconium aspiration syndrome with porcine surfactant. Eur J Pediatr 1996;155:1047-1051.
- 41. Hallmann M, Kankaanpaa K. Evidence of surfactant deficiency in persistence of the fetal circulation. Eur J Pediatr 1980;134:129-34.
- 42. Hallman M. Molecular interactions between nitric oxide and lung surfactant. Biol Neonate 1997;71:44-8.
- 43. Hintz SR, Suttner DM, Sheehan AM, et al: Decreased use of neonatal extracorporeal membrane oxygenation (ECMO): how new treatment modalities have affected ECMO utilization. Pediatrics 2000 Dec; 106(6): 1339-43.
- 44. Holm BA, Notter RH, Finkelstein JN. Surface property changes from interactions of albumin and with natural lung surfactant extracted lung lipids. Chem Phys Lipids 1985;38:287-98.
- 45. Holm BA, Notter RH. Effect of hemoglobin and red blood cell membrane lipids on the biophysical and physiological activity of pulmonary surfactant. J Appl Physiol 198; 63:1434-42.
- 46. Ibara S, Ikenoue T, Murata Y, et al: Management of meconium aspiration syndrome by tracheobronchial lavage and replacement of surfactant TA. ACTA Paediatr Japonica 1995;37:64-67.
- 47. Issa A, Lappalainen U, Kleinman M, Bry K, Hallman M. Inhaled nitric oxide decreases hyperoxia-induced surfactant abnormality in preterm rabbits. Pediatr Res 1999;45:247-54.
- 48. Ivy DD, Kinsella JP, Ziegler JW, Abman SH. Dipyridamole attenuates rebound pulmonary hypertension after inhaled nitric oxide withdrawal in postoperative congenital heart disease. J Thorac Cardiovasc Surg 1998;115:875-82.
- 49. Kanto WP Jr, Bunyapen C: Extracorporeal membrane oxygenation. Controversies in selection of patients and management. Clin Perinatol 1998 Mar; 25(1): 123-35.
- 50. Karamanoukian HL, Glick PL, Zayek M, Steinhorn RH, Zwass MS, Fineman JR, et al. Inhaled nitric oxide in congenital hypoplasia of the lungs due to diaphragmatic hernia or oligohydramnios. Pediatrics 1994;94:715-8.
- 51. Khammash H, Perlman M, Wojtulewicz J, Dunn M: Surfactant therapy in full-term neonates with severe respiratory failure. Pediatrics 1993;92:135-139.
- 52. Konduri GG, Garcia DC, Kazzi NJ, Shankaran S. Adenosine infusion improves oxygenation in term infants with respiratory failure. Pediatrics 1996;97(3):295-300.
- 53. Kinsella JP, Neish SR, Shaffer E, Abman SH. Low-dose inhalational nitric oxide in persistent pulmonary hypertension of the newborn. Lancet 1992;340:819-20.
- 54. Kinsella JP, McQueston JA, Rosenberg AA, Abman SH. Hemodynamic effects of exogenous nitric oxide in ovine transitional pulmonary circulation. Am J Physiol 1992;262:H875-880.
- 55. Kinsella JP, Neish SR, Ivy DD, et al. Clinical responses to prolonged treatment of persistent pulmonary hypertension of the newborn with low doses of inhaled nitric oxide. J Pediatr 1993;123:103-8.
- 56. Kinsella JP, Abman SH. Efficacy of inhalational nitric oxide therapy in the clinical management of persistent pulmonary hypertension of the newborn. Chest 1994;105:92-94S.
- 57. Kinsella JP, Abman SH. Recent developments in the pathophysiology and treatment of persistent pulmonary hypertension of the newborn. J Pediatr 1995;126:853-64.
- 58. Kinsella JP, Torielli F, Ziegler JW, et al. Dipyridamole augmentation of response to NO. Lancet 1995; 346:647-8.
- 59. Kinsella JP, Abman SH. Clinical approach to the use of high frequency oscillatory ventilation in neonatal respiratory failure. J Perinatol 1996;16:S52-55.
- 60. Kinsella JP, Truog WE, Walsh WF, et al. Randomized, multicenter trial of inhaled nitric oxide and high frequency oscillatory ventilation in severe persistent pulmonary hypertension of the newborn. J Pediatr 1997;131:55-62
- 61. Kinsella JP, Abman SH: Inhaled nitric oxide: current and future uses in neonates. Semin Perinatol 2000 Dec; 24(6): 387-95.
- 62. Knight GR, Dudell GG, Evans ML, Grimm PS. A comparison of venovenous and venoarterial extracorporeal membrane oxygenation in the treatment of neonatal respiratory failure. Critical Care Medicine 1996; 24(10):1678-83.
- 63. Lam BC, Yeung CY. Surfactant Lavage for Meconium Aspiration Syndrome: A Pilot Study. Pediatrics 1999. 103(5) Part 1 of 2:1014-1018.
- 64. Levin DL, Heymann MA, Kitterman JA, et al. Persistent pulmonary hypertension of the newborn. J Pediatr 1976;89:626-30.
- 65. Lotze A, Whitsett JA, Kammerman LA, Ritter M, Taylor GA, Short BL. Surfactant protein A concentrations in tracheal aspirate fluid from infants requiring extracorporeal membrane oxygenation. J Pediatr 1990;116:435-40.
- 66. Lotze A, Knight GR, Martin GR, Bulas DI, Hull WM, O’Donnell RM, et al. Improved pulmonary outcome after exogenous surfactant therapy for respiratory failure in term infants requiring extracorporeal membrane oxygenation. J Pediatr 1993;122:261-8.
- 67. Lotze A, Stroud CY, Soldin SJ. Serial lecithin/sphingomyelin ratios and surfactant/albumin ratios in tracheal aspirates from term infants with respiratory failure receiving extracorporeal membrane oxygenation. Clin Chem 1995;41:1182-8.
- 68. Lotze A, Mitchell BR, Bulas DI, et al: Multicenter study of surfactant (beractant) use in the treatment of term infants with severe respiratory failure. Survanta in Term Infants Study Group. J Pediatr 1998 Jan; 132(1): 40-7.
- 69. Luce, JM: Acute lung injury and the acute respiratory distress syndrome. Crit Care Med 1998;26(2):369-376
- 70. Marks, Stephen D. MBChB, MRCP(UK), DCH, MRCPCH. Nicholl, Richard M. MBChB, MRCP(UK), DCH, MRCPCH. The reduction in the need for ECMO by using surfactant in meconium aspiration syndrome. J Pediatr. 135 1999;267-268.
- 71. Morin FC 3rd, Stenmark KR: Persistent pulmonary hypertension of the newborn. Am J Respir Crit Care Med 1995 Jun; 151(6): 2010-32.
- 72. Moses D, Holm BA, Spitale P, Liu M, Enhorning G. Inhibition of pulmonary surfactant function by meconium. Am J Obstet Gynecol 1991;164:477-81.
- 73. Neonatal Inhaled Nitric Oxide Study Group. Inhaled nitric oxide in full-term and nearly full-term infants with hypoxic respiratory failure. N Engl J Med 1997;336:597-604.
- 74. Neonatal Inhaled Nitric Oxide Study Group. Inhaled nitric oxide and hypoxic respiratory failure in infants with congenital diaphragmatic hernia. Pediatrics 1997;99:838-45.
- 75. O’Donnell VB, Chumley PH, Hogg N, Bloodworth A, Darley-Usmar VM, Freeman BA. Nitric oxide inhibition of lipid peroxidation: kinetics of reaction with lipid peroxyl radicals and comparison with alpha-tocopherol. Biochemistry 1997;36:15216-23.
- 76. Oka M, Ohnishi M, Takahishi H, Soma S, Hasunuma K, Sato K, et al. Altered vasoreactivity in lungs isolated from rats exposed to NO gas. Am J Physiol 1996;271:L419-24.
- 77. Paranka MS, Walsh WF, Stancombe BB. Surfactant lavage in a piglet model of meconium aspiration syndrome. Pediatr Res 1992;31:625-8
- 78. Paranka MS, Clark RH, Yoder BA, Null DM Jr: Predictors of failure of high-frequency oscillatory ventilation in term infants with severe respiratory failure. Pediatrics 1995 Mar; 95(3): 400-4.
- 79. Patole SK, Finer NN. Experimental and clinical effects of magnesium infusion in the treatment of neonatal pulmonary hypertension. Magnesium Research 1995;8(4):373-88, 1995.
- 80. Robbins CG, Davis JIM, Merritt TA, et al. Combined effects of nitric oxide and hyperoxia on surfactant function and pulmonary inflammation. Am J Physiol 1995;272:L545-550.
- 81. Roberts JD, Polaner DM, Lang P, Zapol WM. Inhaled nitric oxide in persistent pulmonary hypertension of the newborn. Lancet 1992;340:818-9.
- 82. Roberts JD, Chen TY, Kawai N, Wain J, Dupuy P, Shimouchi A, et al. Inhaled nitric oxide reverses pulmonary vasoconstriction in the hypoxic and acidotic newborn lamb. Circ Res 1993;72:246-54.
- 83. Roberts JD Jr, Fineman JR, Morin FC 3rd, et al: Inhaled nitric oxide and persistent pulmonary hypertension of the newborn. The Inhaled Nitric Oxide Study Group. N Engl J Med 1997; 336(9): 605-10.
- 84. Rossaint R, Falke KJ, Lopez F, Slama K, Pison U, Zapol WM. Inhaled nitric oxide for the adult respiratory distress syndrome. N Engl J Med 1993; 328: 399-405.
- 85. Rotta AT, Gunnarsson BJ, Guhrman BP, et al. Comparison of lung protective ventilation strategies in a rabbit model of acute lung injury. Crit Care Med, Volume 29(11).November 2001.2176-2184.
- 86. Roy BJ, Rycus, P, Conrad SA, Clark RH. The Changing Demographics of Neonatal Extracorporeal Membrane Oxygenation Patients Reported to the Extracorporeal Life Support Organization (ELSO) Registry. Pediatr 2000; 106(6):1334-1338.
- 87. Royal JA, Levin DL. Adult respiratory distress syndrome in pediatric patients. I. Clinical aspects, pathophysiology, pathology, and mechanisms of lung injury. J Pediatr 1988;112:169-80.
- 88. Seeger W, Stohr G, Wolf HRD, Neuhof H. Alteration of surfactant function due to protein leakage: special interaction with fibrin monomer. J Appl Physiol 1985;58:326-38.
- 89. Soll, RF; Dargaville, P. Surfactant for meconium aspiration syndrome in full term infants. The Cochrane Database of Systematic Reviews Volume (Issue 4).2000.
- 90. Steinhorn RH, Millard SL, Morin FC 3rd: Persistent pulmonary hypertension of the newborn. Role of nitric oxide and endothelin in pathophysiology and treatment. Clin Perinatol 1995 Jun; 22(2): 405-28.
- 91. Stevenson DK, Kasting DS, Darnall RA, et al. Refractory hypoxemia associated with neonatal pulmonary disease: the use and limitations of tolazoline. J Pediatr 1979;95:595-9.
- 92. Sun B, Curstedt T, Robertson B. Surfactant inhibition in experimental meconium aspiration. Acta Paediatr 1993;82:182-9.
- 93. Sun B, Curstedt T, Song G-W, Robertson B. Surfactant improves lung function and morphology in newborn rabbits with meconium aspiration. Biol Neonate 1994;63:96-104.
- 94. Tworetzky W, Bristow J, Moore P, et al: Inhaled nitric oxide in neonates with persistent pulmonary hypertension. Lancet 2001 Jan 13; 357(9250): 118-20.
- 95. UK collaborative randomised trial of neonatal extracorporeal membrane oxygenati: UK Collaborative ECMO Trail Group. Lancet 1996 Jul 13; 348(9020): 75-82.
- 96. Walsh-Sukys MC, Tyson JE, Wright LL, et al: Persistent pulmonary hypertension of the newborn in the era before nitric oxide: practice variation and outcomes. Pediatrics 2000 Jan; 105(1 Pt 1): 14-20.
- 97. Ware LB, Matthay MA. The Acute Respiratory Distress Syndrome. N Engl J Med, Volume 342(18).May 4, 2000.1334-1349.
- 98. Weigand MA, Snyder-Ramos SA, Bauer J, et al. Inhaled nitric oxide does not enhance lipid peroxidation in patients with acute respiratory distress syndrome. Crit Care Med 2000, Volume 28(10):3429-3435.
- 99. Wessel DL, Adatia I, Van Marter LJ, et al. Improved oxygenation in a randomized trial of inhaled nitric oxide for persistent pulmonary hypertension of the newborn. Pediatrics 1997;100:e7.
- 100.Wiswell, TE. The Surfaxin-Lavage for MAS Trial Group. Bronchoalveolar Lavage with Dilute SurfaxinTM (KL4-Surfactant) for the Management of the Meconium Aspiration Syndrome. Pediatric Research 1999. 45(4) Part 2:326A.
- 101.Wolfson MR, Greenspan JS, Shaffer TH. Pulmonary administration of vasoactive substances by perfluorochemical ventilation. Pediatrics 1996;97:449-55.
- 102.Wung JT, James LS, Kilchevsky E, James E: Management of infants with severe respiratory failure and persistence of the fetal circulation, without hyperventilation. Pediatrics 1985 Oct; 76(4): 488-94.
- 103.Ziegler JW, Ivy DD, Kinsella JP, Abman SH: The role of nitric oxide, endothelin, and prostaglandins in the transition of the pulmonary circulation. Clin Perinatol 1995 Jun; 22(2): 387-403.
- 104.Ziegler JW, Ivy DD, Wiggins JW, et al. Effects of dipyridamole and inhaled nitric oxide in pediatric patients with pulmonary hypertension. Am J Respir Crit Care Med 1998;158:1388-95.