Drenaje Torácico Desafiante: Reporte de un Caso
Challenging Chest Drainage: A Case Report
Abstract
Introduction. Chest trauma is one of the most common causes of death corresponding to 20 to 25 % of cases. The majority of the patients (85%), can be managed with only a tube thoracostomy.
Our objective by presenting this case report is to provide an example of how to manage a challenging chest tube thoracostomy in a patient with cardiac hernia diagnosed in the preoperative phase, based on signs of computed tomography.
Case report. A 45-year-old male presented to our emergency department who fell from a light pole 7 meters high. He fell to the ground on his back. Physical examination revealed a huge subcutaneous emphysema on his entire anterior chest wall and presented no sensitivity or movements below the navel line. After the initial assessment and management care, the patient improved.
As the patient stabilized we decided to go to CT. The scan revealed pericardial rupture with only the right pericardial circumference intact, the heart herniated into the left pleural space, bilateral pneumothorax, small right hemothorax and a relevant subcutaneous emphysema surrounding the chest.
We decided to perform the blunt dissection technique to insert chest tubes bilaterally because of safety. After performed it the patient was transferred to cardiothoracic department.
Discussion. There is a variety of techniques to perform tube thoracostomy but the blunt dissection remain the safer, especially when we are facing an anatomic distortion of the heart.
Conclusion. We present a case report of a challenging thoracic drainage performed in a patient with traumatic cardiac hernia, which procedure was successful.
Keywords: thoracic injuries; wounds, nonpenetrating; heart injuries; myocardial contusions; chest tube; thoracos- tomy.
Resumen – Drenaje Torácico Desafiante
Introducción. El traumatismo torácico es una de las causas más comunes de muerte y corresponde al 20 a 25 % de los casos. La mayoría de los pacientes (85 %) pueden tratarse solo con toracostomía.
Nuestro objetivo al presentar este informe de caso es proporcionar un ejemplo de cómo manejar una toracostomía desafiante en un paciente con hernia cardíaca, diagnosticada en la fase preoperatoria, basada en signos de tomografía computarizada.
Presentación del caso. Paciente masculino de 45 años que ingresa a nuestro departamento de emergencias luego de caída de 7 metros de altura (poste de luz), cayendo de espaldas al suelo.
El examen físico reveló un enfisema subcutáneo importante en todo el tórax anterior y sin sensibilidad ni movimientos debajo de la línea del ombligo.
Después de la evaluación y atención inicial el paciente mejoró y se decidió realizar una tomografía computarizada que reveló la rotura pericárdica, con solo la circunferencia pericárdica derecha intacta, el corazón herniado en el espacio pleural izquierdo, neumotórax bilateral, pequeño hemotórax en el lado derecho y enfisema subcutáneo rodeando completamente el tórax.
Se escogió una técnica de disección roma para insertar el tubo torácico en ambos hemitórax, debido a su mayor seguridad. Posteriormente, el paciente fue trasladado al departamento de cirugía cardiotorácica.
Discusión. Existe una variedad de técnicas para realizar una toracostomía con sonda, pero la disección roma sigue siendo la más segura, especialmente cuando enfrentamos una distorsión anatómica del corazón.
Conclusión. Presentamos el caso de un drenaje torácico desafiante practicado a un paciente con hernia cardíaca traumática, con éxito.
Palabras clave: lesiones torácicas; heridas no penetrantes; lesiones cardíacas; contusiones miocárdicas; tubos de tórax; toracostomía.
Introduction Chest trauma is one of the most common causes of death, accounting for 20 to 25% of cases1 . It can be due to blunt or penetrating trauma. Most patients (85%), can be treated with just a closed chest drainage, and only 10 to 15% of these patients will need an emergency thoracotomy2 .
Cardiac hernia is a rare clinical condition, diagnosis based on clinical findings, and even through suggestive signs on computed tomography is very difficult, and can be neglected in the preoperative period very easy3 .
Our objective in this case report is to present an example of how to perform a challenging thoracic drainage in a patient with cardiac hernia diagnosed preoperatively, based on computed tomography findings.
Case report – Drenaje Torácico Desafiante
A 45-year-old male was brought to our emergency service by the emergency medical service – SAMU, immobilized on a rigid board and cervical collar. The patient fell down from a 7-meter-high lamp post hitting the ground on his back.
On arrival he was complaining of shortness of breath, confused, with blood pressure (BP) of 110/70 mmHg, heart rate of 115 beats/min, respiratory rate of 25 breaths/min, and oxygen saturation of 97%.
The physical examination revealed:
a. Pervious airways, without neck pain;
b. Swollen chest; on palpation a subcutaneous emphysema throughout the anterior chest wall was observed; breath sounds slightly decreased bilaterally;
c. Flat and flaccid abdomen, negative FAST in all three abdominal regions, the cardiac site was unable to visualize due to subcutaneous emphysema; pelvis stable, with no signs of external bleeding;
d. Glasgow 14 (lost point in verbal response); isochoric pupils and photo reactive;
e. No deformities in the upper and lower limbs, clear on his back, and no sensitivity or movements below the navel line.
Supplemental oxygen was indicated through a mask with an oxygen reservoir, 500 ml of warm crystalloids were administered, and blood samples for hemoglobin/hematocrit and blood typing were collected. After the evaluation and initial care, the patient showed signs of improvement with a reduction in his heart and respiratory rate to normal values.
As the patient became stable, was taken to the imaging suite to perform a CT scan to look which side of the chest was the source of the pneumothorax and subcutaneous emphysema.
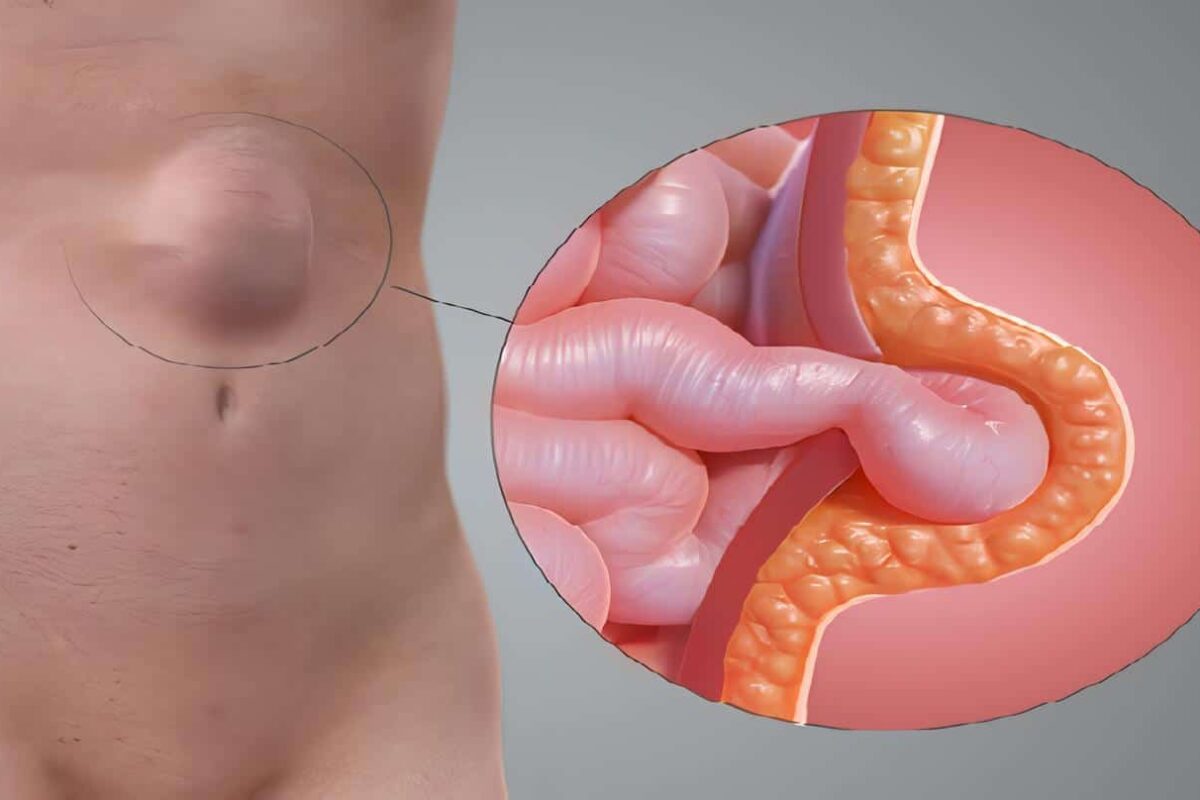
Computed tomography revealed a pericardial rupture with only the right pericardial circumference intact, hernia of the heart to the left pleural space, bilateral pneumothorax, small hemothorax on the right, and a subcutaneous emphysema around the entire chest (Figures 1-2).

Figure 1. Right hemothorax, cardiac herniation to the left pleural space and right branch of pericardium intact.

Figure 2. Bilateral pneumothorax, cardiac herniation to the left pleural space, and subcutaneous emphysema.
Which surgical technique should the team use to drain both pleural cavities? It was decided to perform the chest drainage by blunt dissection as it is a safer technique.
During the procedure on the left side it was possible to feel the “impressions” of the coronary arteries and the right ventricle, the tube was carefully passed in the posterior and superior direction. Air outlet was observed (Figure 3).

Figure 3. On palpation of the pleural cavity it was possible to felt the cardiac structures.
On the right side there was an outflow of air and 300 ml of bloody output.
Then the patient was transferred to the department of thoracic surgery and neurosurgey. He underwent left thoracotomy and was diagnosed with paraplegia. Recovery well after thoracic surgery.
Discussion – Drenaje Torácico Desafiante
There are a variety of techniques to perform a chest drainage, based on the insertion method, such as the Seldinger technique and trocar insertion, which is faster, smaller incision, and there is a minimal tissue dissection resulting in less pain, as smaller drains’ caliber are used, with even better aesthetic results4 .
The Seldinger technique is used by several services for draining both small liquid and gaseous collections, the main disadvantage is the inability to digitally palpate the pleural cavity and the difficulty of correctly directing the position of the chest tube5 .
The trocar insertion technique is performed with a wire passed inside the chest drain, a small incision is made in the skin and the trocar/drain set is inserted towards the pleural cavity.
Although several authors considered a very simple technique, we do not recommend it due to the risk of lesion of the lung and adjacent organs6,7.
Cardiac injury can happen during the thoracic drainage but is very rare and a catastrophic complication.
Most of these injuries are related to anatomical distortion of the thoracic organs, as after pneumonectomy, extreme kyphoscoliosis, and cardiomegaly7-9.
One of these iatrogenic cardiac injuries was related to cardiomegaly and the procedure was performed using the Seldinger technique10.
In the case presented, was preferred the blunt dissection technique, as the team was facing an anatomical distortion of the heart (cardiac hernia) due to thoracic trauma, as it is the safest method and has the advantage of palpating the pleural cavity during the procedure.
Some of these patients with small or moderate traumatic pneumothorax, in the absence of other significant injuries or need for positive pressure, could be treated conservatively.
This was the opposite in our patient that had cardiac herniation to the left pleural space and hemothorax in the right side11.
Thoracic drainage is a simple and the most used procedure in thoracic surgery. Blunt dissection is the oldest technique; it is considered very painful, and some authors report that 50% of patients report pain in 9 out of 10 on a scale of 10 12.
This is still the only technique that allows palpation of the pleural cavity, to assess the presence of loculations, adequate drain position, palpation of adjacent organs in situations of anatomical distortion and especially when vital organs in the chest could not be confirmed before the drain insertion with imaging methods13.
Conclusion – Drenaje Torácico Desafiante
Learning the correct technique, the right indication, recognizing possible complications that may occur, and how to deal with these complications is essential for doctors working in urgent and emergency services.
We present a case of challenging thoracic drainage in which the anatomic distortion of the heart caused by a cardiac herniation to left pleural space could be diagnosed before the insertion of the chest tube.
Compliance with ethical standards
Informed consent: Informed consent was obtained from the patient.
Conflict of interest: None.
Funding: Financed with author resources.
Contribution of the authors: The author declares to have contributed in their entirety in the realization of the work.
References – Drenaje Torácico Desafiante
1. Carver DA, Bressan AK, Schieman C, Grondin SC, Kirk- patrick AW, Lall R, et al. Management of haemotho- races in blunt thoracic trauma: study protocol for a randomised controlled. BMJ Open. 2018;8:e020378. http://dx.doi.org/10.1136/bmjopen-2017-020378
2. Mattox KL, Wall MJ, Tsai P. Trauma thoracotomy: principles and techniques In: Mattox KL, editor; Moore EE, editor; Feliciano DV, editor. (eds). Trauma, 7th edn New York: McGraw-Hill, 2013; 461-467.
3. Lindenmann J, Matzi V, Neuboeck N, Porubsky C, Rat- zenhofer B, Maier A, Smolle-Juettner JM. Traumatic pericardial rupture with cardiac herniation. Ann Thorac Surg. 2010;89:2028-30. http://doi.org/10.1016/j.athoracsur.2009.10.048
4. Mahmood, K. Wahidi MM. Straghtening out chest tubes: what size, what type and when. Clin Chest Med. 2013;34:63-71. http://doi.org/10.1016/j.ccm.2012.11.007
5. Havelock T, Teoh R, Laws D, Gleeson F, BTS Disease Guideline Group. Pleural procedures and thoracic ultrasound: British thoracic Society pleural disease guideline 2010. Thorax. 2010;65(Suppl 2):ii61-76. https://doi.org/10.1136/thx.2010.137026
6. Fraser RS. Lung perforation complicating tube thoracostomy: pathologic description of three cases. Hum Pathol. 1988;19:518-23. https://doi.org/10.1016/s0046-8177(88)80197-7
7. Meisel S, Ram Z, Priel I, Nass D, Lieberman P. Another complication of thoracostomy perforation of the right atrium. Chest. 1990;98:772-3. https://doi.org/10.1378/chest.98.3.772
Bibliography – Drenaje Torácico Desafiante
8. Kopec SE, Conlan AA, Irwin RS. Perforation of the right ventricle: a complication of blind placement of a chest tube into the postpneumonectomy space. Chest. 1998;114:1213-5. https://doi.org/10.1378/chest.114.4.1213
9. Al aseri Z. Accuracy of chest radiograph interpretation by emergency physicians. Emerg Radiol. 2009;16:111-4. https://doi.org/10.1007/s10140-008-0763-9
10. Kim D, Lim SH, Seo PW. Iatrogenic perforation of the left ventricule during insertion of a chest drain. Korean J Thorac Cardiovasc Surg. 2013;46:223-225. https://doi.org/10.5090/kjtcs.2013.46.3.223
11. Correa-Restrepo J, Restrepo-Moreno M, Peláez LG, Díaz-Cadavid RD, López-Vasco Y, Rojas MA, et al. Radiografía de tórax de control en pacientes con neumotórax postraumático asintomático. Rev Colomb Cir. 2020;35:75-83. https://doi.org/10.30944/20117582.590
12. Kuhajda I, Zaragoulidis K, Kougioumtzi I, Huang H, LI Q, Dryllis G, et al. Tube thoracostomy; chest tube implantation and follow up. J Thorac Dis. 2014;6(Suppl 4): S470-S479. https://doi.org/10.3978/j.issn.2072-1439.2014.09.23
13. American College of Surgeons (ACS) (United States). ATLS Advanced Trauma Life Support: student course manual. 10.ed. Chigago: The Committee On Trauma, 2018.
Autor – Drenaje Torácico Desafiante
Bruno José da Costa Medeiros, General surgeon, Instituto de Cirurgia do Estado do Amazonas – ICEA; Manaus, Brasil
Received date: 07/07/2020 – Acceptance date: 09/17/2020 – Published online: 04/06/2021
Corresponding author: Bruno José da Costa Medeiros. Estado do Amazonas – ICEA; Manaus, AM 69053610. Phone number: 5592984490880. Email: brunaojose@bol.com.br
Cite as: da Costa Medeiros BJ. Challenging chest drainage: a case report. Rev Colomb Cir. 2021;36:540-4. https://doi.org/10.30944/20117582.711
This is an open access article under a Creative Commons License – BY-NC-ND https://creativecommons.org/licenses/by-ncnd/4.0/deed.es