Estadísticamente se ha observado que un 10% de los pacientes con hiperinsulinismo tienen un síndrome MEN 1. El insulinoma es el segundo tumor funcionante de células de los islotes más común en este síndrome familiar. La presencia de un MEN I puede ser determinada por una cuidadosa historia familiar y la búsqueda de otras manifestaciones del síndrome. Los niveles precisos en el suero de calcio, prolactina y polipéptidos pancreáticos pueden ser útiles para detectar su presencia (87, 88).
El páncreas de pacientes con síndrome MEN 1, siempre tienen múltiples tumores de los islotes pancreáticos, y los estudios recientes sugieren que el duodeno también tiene múltiples tumores neuroendocrinos (87-89). Sin embargo, estudios cuidadosos con inmunoperoxidasa hacen ver que los tumores pancreáticos son insulinomas (90). Otro hecho importante es que los grandes tumores pueden ser malignos. Los pacientes con MEN I e insulinoma, generalmente tienen un tumor de las células de los islotes dominante, capaz de ser localizado por imágenes y ser el responsable de la excesiva secreción de insulina, además de la identificación de otros tumores pequeños. Si el tumor dominante está presente dentro del cuerpo o la cola del páncreas, se recomienda una pancreatectomía distal o subtotal. Si el tumor dominante está en la caheza pancreática, se de he intentar la enucleación. Si esto no es posible y el tumor es grande y está en la cercanía del canal principal, existe indicación para la pancreatoduodenectomía.
No obstante el hecho de que estos pacientes tienen múltiples tumores de los islotes y que algunos pueden ser malignos, ellos permanecen libres de hipoglicemia después de la resección quirúrgica. Se requiere un cuidadoso seguimiento debido a que puede desarrollarse un hiperinsulinismo recurrente ya sea por la recurrencia de otro insulinoma o por desarrollo de enfermedad metastásica del tumor original. Las resecciones quirúrgicas repetidas están indicadas para el hiperinsulinismo recurrente en pacientes con MEN 1, SI el procedimiento conlleva aceptable morbimortalidad.
La presencia de otras endocrinopatías como el hiperparatiroidismo primario en pacientes con MEN J, puede afectar los síntomas relacionados con los tumores de los islotes; por lo tanto, se recomienda eliminar por cirugía primero el hiperparatiroidismo primario, para mejorar el control del tumor de células insulares.
Abstract
With the presentation of 8 cases of benign insulinomas, a review of current concepts on gastroenteropancreatic neuroendocrine tumor, is made. With relation to insulinomas, alfention is ml/ed upon fasting hypoglicemia. emphasiúng that this one is more severe than other causes of low blood sugar, always implicating. in adults. a high degree (of hyperinsulinism. Complementan” laboraton” studies are also of great importanCe for the recognition of the inappropriate secretion of insulin and other pancreatic peptides, through the concomitant elevation of plasmatic glucose and insulin; thus establishing the circulating insulin/ilucose ratio.
Emphasis is made on the use of se!ective arteriography and intra-operatory ultrasonographv for the diagnosis of insulin secreting tumors. The first method offers the greatest sensibility for localization of the tumor and the lalfer is (j{ great use when preoperative imageneological studies are inconc/usive. speciallv with ven” smal/ tumors.Finally. the complete enuc/eation o{ the insulinoma is underlined as the best technique for extirpation of this type of benign tumor, obtaining through it a high percentage of svmptomatic improvement.
Referencias
l. Filipi C J, Higgins G A: Diagnosis and management 0f insulinoma. Am J Surg 1973; 125: 231-8
2. Stefanini P. Carbonari M, Patrassi N et al: Beta-islet cel1 tumors of the pancreas: Results 0f a study on I .067 cases. Surgery 1974; 75: 597-607
3. Buchanam K D. Johnston C F. O’Hare N M T et al: Neuroendocrine tumors. a European view. Am J Med 1986; 81: 14-•22
4. Whiple A O, Franlz V K: Adenoma of’ lhe islet eell with hiperinsulinism. Ann Surg 1935; 10 1: 1299-1305
5. Whiple A O: Surgery of the pancreas. In: The Evolution of Surgery in the United States. Springl’ield. 1II. Charles C Thomas. 1963; pp. 138-45
6. Alfidi R J. Bhyun D S, Crilc G Jr et al: Arteriography and hypoglycemia. Surg GynecolObstet 1971; 133: 447-52
7. Fraker D L. Norton J A: Localization and resection 01′ insulinoma and gastrinomas. JAMA 1988; 259: 3601-5
8. Dunnick N R. Long J A. Krudy el al: Localizing insulinomas with comhined radiographic methods. Am J Roentgenol 1980; 135: 747-52
9. Comi R J. Gorden P, Doppman H L, Norton J A: Insulinoma. In: GoVLM. Gardner J D, Brooks F P el al, eds. The exocrine pancreas: hiology pathology and diseases. New York: Raven Press. 1986; pp. 745-61
10. Service F J, Horwitz D L. Ruhenstein A H et al: C-peptide suppression test for insulinoma. J Lah Clin Med 1977; 99: 180-6
11. Harrison T S. Child C G, Fry W J ct al: Current Surgical management of functioning islel cell tumors of the pancreas. Ann Surg 1973; 178: 485-91
12. O’Neal L W. Kipnis D M, Luce S A et al: Secrelion 01′ various endocrine substances hy ACTH-secreting tumors: Gastrin melanotropin. serotonina. parathormonc, vasopressin. glucagon. Cancer 1968: 21: 1219-28
13. Dayal Y: Neuroendocrine cells of the gastroinlestinal tract: Introduction and historical perspective. In: Endocrine Pathology of the Gut and Pancreas. Edited hy Y Dayal. 1991; pp. 1-31. Boca Raton, Florida.
14. Kultschitzky N: Zul’ I’rage uher den Baudes Darmkanals. Arch Mikrosk Anat 1897; 49: 7-35
15. Ciaccio C: Sur nouvelle espece cellulaire dans les glandes de Lieherkuhn. Compt Rend Soc Biol, Paris. 1906: 60: 76-8
16. Hehschmann P: Sur le carcinome primitif de I’appendice vcnnicularie. Rev Med Suisse Romande. 1910; 10: 317-32
17. Gossct A, Masson P: Tumeurs endocrines dc I’appendice. Presse Med 1914; 22: 237-40
18. Feyrter F: Veher dil”l”use endokrine Organe. Zhl Inn Med 1938; 59: 545-52
19. Pearse A: Common cytochemical and ultracstructural characteristics of cells producing polypeptide hormones (the APUD series) and their relevance to thyroid and ultimo hranquial C cells and calcitonin. Proc R Soc B 1968; 170: 71-80.
20. Pearse A G: The cytochemistry and ultraeslructure of polypeptide hormone producing cells of’ lhe APUD series and the emhryologic and pathologic Implications of lhe concept. J Histochem Cylichem 1969: 17: 303-13
21. Mozell E. Woltering E. Stenzel P et al: Functional endocrine tumors of the pancreas: Clinieal presentation, diagnosis. and trealment. Curr Prohl Surg 1990: 303-86
22. Kerr D 1, Burt A D, Anderson J R. Tumours 01″the dil”l”erent endocrine System. Eur J Surg Oncol 1987; 13: 189-95
23. Andrew A: Further evidence that enlerochromafl”in cells are not derived from the neural erest. J Embryol 1987; 13: 189-95
24. Dawson 1: Dil”l”use endocrine and neuroendocrine cell tumours. In: Recent Advances in Histopathology. Edited by P.P. Anthony and R.N.M. Me Sween. Vol. XII. Edinhurgh: Churchill Livingstone Inc. 1984
25. Pearse A G E: Genesis 01′ the neuroendocrine system. In: Surgieal Endoerinology. Edited hy S.R. Friesen and N. W. Thompson. Philadelphia J. B. Lippincott Co. 1990: pp. 15-21
26. Le Durain N: On the origin of pancrealic endocrine cells. 1988; 53: 169-71
27. Dchas H T: Clinical signil”icance of gastrointestinal hormones. Adv Surg 1987; 21: 157-88
28. Krejs G J: Gastrointestinal Endocrine tumors. Am J Med 1987; 82: 1-3
29. Solcia E, Capella C, Fiocca R et al: The gastrocntcropancrcatic endocrinc systcm and related tumors. Gastroenterol Clin North Am 1989; 18: 671-92
30. Wilder R M, Allan P H. Power M H et al: Carcinoma 01″ the islands of the pancreas. Hyperinsulinism and hypoglycemia. JAMA 1927; 89: 348-54.
31. Graham R R: Quoted in: G Howland, W R Camppe!. E 1 Malthy et al: Dysinsulism: Convulsions ami coma due to islet-cell tumor of the pancreas with operation and cure. lAMA 1929: 93: 674-9
32. Berger M, Borde e. Cupper H el al: Functional and Morphologic charactcrization of hutnan insulinomas. Diahetes 1983; 32: 921-6
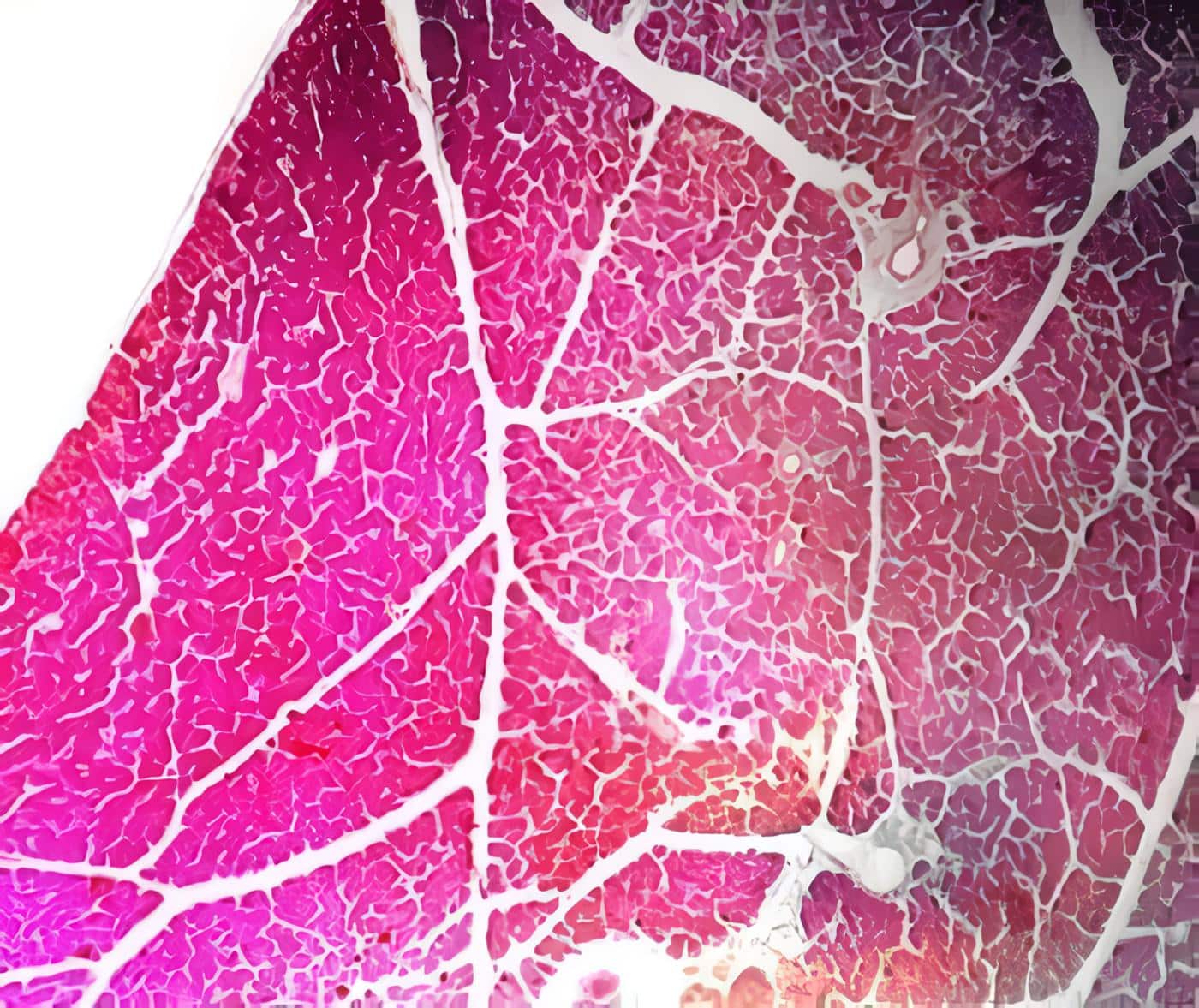
33. Heitz P U, Kloppel G, Hacki W H et al: Nesidiohlaslosis: The pathologic hasis of persistent hiperinsulincmia hypogliccmia in infants: Morphologic and LJuantitative analysis of seven cases hased spccific ill1ll1unostaining and electrol1 microscopy. Diahetes 1977: 26: 632-42.
34. Harness 1 K. Geelhoed G W. Thompson N W et al: Nesidiohlastosis in adults. A surgical dilema. Arch Surg 1981; 116: 675-580
35. Harrison T S, Fajans S S. Floyd 1 C J r et al: Prevalenee 01′ difuse pancreatic heta islet eell disease with hyperinsulinism-prohlems in recognition and managemcnt. World 1 Surg 1984; 8: 583-9
36. Nathan D M. Axelrod L. Proppe K H et al: NesidiobhLstosis associated with insulin mcdiated hipoglicemia in an adult. Diabetes Care 1981; 4: 383-8
37. Dclgado 1 e. Castro 1 E. Landazáhal G, Matiz E: Nesidiohlastosis en adultos. Rev Col Cirug. 1984; 9; 193-200
38. Stefanni P, Carhoni M, Patrassi N ct al: Beta-islet cell tumors 01′ thc pancreas: Results 01′ a sludy on 1.067 cases. Surgery 1974; 75: 597-609
39. Case records 01′ the Massachusetts General Hospital. Weekly clinieopathologieal exereises. Case 30. N Engl 1 Med 1978; 299: 241-56
40. Jaffe R. Hashida y, Yunis E J: Pancreatie pathology in hyperinsulinemic hypoglyeemia of infancy. Lah Invest 1980; 42: 356-65
41. Marks V: The measurement of hlood glucose and the dcfinition of hypoglyeemia: Procceding of the Rome Symposium. Stuttgart, Georg Thieme Verlag 1976; p. 1
42. Serviee F 1; Hypoglycemic Disorders. Boston, G K, Hall Medical Puhlishers. 1983
43. Rihalet B, Biegelman P: Calcium Potencials and potassium permeahility activation in panereatic B cells. Am J Physiol 1980; 139: 124-9
44. Siegel E, Creutzfeldt W: Stimulation of insulin release in isolated rat islets hy GIP in phisiological concentrations and its relation to islet eell cyclic AMP content. Diahetalogía 1985; 28; 857-61
45. Anderson D, Elahi D, Brown J et al: Oral glucose augmcntatioll of insulin secretion. Illteractions of gastric inhihitory polypeptide with ambient glucose and insulin levcls. 1 Clin Invest 1978; 62: 152-8
46. Comi R 1. Gorden P: Hypoglycemic di sorders in the adult. In: Becker K L (ed); Principies and Practice of Endocrinology and Metabolism. Philadelphia, lB Lippincott, 1990; pp. 1198-205
47. Comi R 1. Gorden p. Doppman 1 L et al: Insulinoma: In: Go YLM (ed): The exocrine Pancreas. New York, Raven Press 1986; pp. 745- 61
48. Unger R: Insulino-glucosa relationship in the derense against hypoglycemia. Diahetes 1983; 32: 575-83
49. Gerich 1 E. Mokaw M. Yeneman T et al; Hypoglycemia anawareness. Endocr Rev 1991; 12: 356-71
50. Scholz D A, Remine W H, Priestly 1 T: Clinics on endocrine and metaholic diseases. 3. Hyperinsulinism. Review of 95 eases of functioning pancreatic islet cell tumors. Mayo Clin Proc 1960; 35: 545-55
51. Ramos E, Zorrilla E, Hadley W B: Fever as a manifestation 01′ hypoglyeemia. J Am Med Assoc 1968; 205: 590-4
52. Gale E A, Bennett T, MacDonald 1 A et al: Responses at diffcring levels of blood glucose. Clin Sci 1983; 65: 263-7
53. Dante G: Hypoglycemia peripheral ncuropathy. Arch Neurol 1969; 21: 121-5
54. Wenzel E, Comi R 1: Use of octreolide in c1inical endocrinology. Endocrinologist 1991; 1: 256-64
55. Doherty G M, Doppman 1 L, Shawker T H, Easman R C, Gorden P, Norton 1 A: Results of a prospecti ve strategy to diagnose, localize and resect insulinoma. Surgery 1991; 11: 989-97
56. Gorden P. Roth 1. Freychet P, Kahn R: The circulating proinsulina Iike components. Diahetes 1972; 21: 673-7
57. Merimee T 1, Tyson 1 E; Stahilization of plasma glucosa during fasting. Normal variations in two separatc studies. N Engl Med 1974; 291: 1275-8
58. Turner R C, Oakley N W, Naharro J D N: Control 01′ basal insulin secretion, with special reference to the diagnosis of insulinomas. Br Med 1971; 11: 132-6.
59. Patiño 1 F: El concepto APUD y los Apudomas. Unificación Patobiológiea de diversas neoplasias endocrinas. En: FEPAFEM 1979; 1-43
60. Rubenstein A H. Kazuya H, Horwitz D L: Clinical significance 01′ circulating Cpeptide in diahetes mellitus and hypoglycemic disorders. Arch Intern Med 1977; 137: 625-32
61. Rubenstein A H. Steiner D F, Horwitz D L: Clinical significanee of circulating proinsulin and C-peptide. Recent Prog Honn Res 1977; 33: 435-40
62. Odell W: Paraendocrine Syndromes of cancel’. Adv Intern Med 1989: 34: 325-31
63. Merience T: Insulin-like growth factors in patienls with non- islet ceIl tumors and hypoglyccmia. Metaholism 1986; 35:360-6
64. Service F. Dale A, Elveback L et al; Insulinoma-Clinical and diagnostic fealures of 60 consecutive cases. Mayo Clin Proc 1976; 51: 417-22
65. Floyd J C. Fajan S S, Knopf R F et al: Plasma insulina in organie hyperinsulinism: Comparative effects of tolhutamide, leucine and glueose. 1 Clin Endocrinol Metab 1964; 24: 247-52
66. Marks Y, Samols E: Glucagon test for insulinoma. A chemical study in 25 cases. 1 Clin Palhol 1968; 2 1: 346-51
67. Kaplan E L, Ruhenstein A H, Evans R et al: Calcium infusion. A new provocative test for insulinomas. Ann Surg 1979; 190: 501-4
68. Glaser B, Shapiro B, Glowniak 1 et al: Effets of secretin on the normal and pathologic heta cel!. 1 Clin Endocrinol Metah 1968; 66: 1138-43
69. Turner R C, Heding L G: Plasma proinsulin, C-peptide and insulin in diagnostic suppression test for insulinomas. Diahetología 1977; 13: 571-7
70. Kahn C R, Rosen S W, Weitraub B D et al: Ectopic production 01′ chorionic gonadotropin and its subunits by islettumors. A specific marker for malignancy. N Engl 1 Med 1977; 297: 565-9
71. Lamherts S W. Hotland L 1: In vivo and in vitro detection of functional somatostatin receptors in human endocrine tumors: conseLJuences with regard to
diagnosis, localization and therapy. J Clin Endocrinol Metab 1990; 3 1: 566-73 72. Caro A: Apudomas pancreáticos: En: Cirugía del Páncreas. Fund OFA (ed). 1984; pp. 195-224
73. Dunnick N, Long 1, Krudy A et al: Localizing insulinomas with combined radiographic methods. A 1 R 1982; 135: 747-51
74. Fulton R, Shcedy P, McIlrath D et al: Preoperative angiographic localization of insulin- producing tumors of the pancreas. A1R. 1975; 123: 367-71
75. Pedrazzolis P, Miotto D et al: Transhepatic portal sampling for preoperative localization 01′ insulinomas. Surg GynecolOhstet 1988; 165: 101-6
76, Rosch T. Lightdale C J. Botet J F ct al: Localization 01′ pancreatic endocrinc tumors by endoscopic ultrasonography. N Eng J Med 1992; 326: 1721-6
77. Grant C S, Van Heerden J, Charboneau J W, James E M, Reading C C: Insulinoma: the value of intraopcrative ultrasonography. Arch Surg 1988; 123:
843-8
78. Norton J A, Shawker T H, Doppman J L et al: Localization and surgical treatment of occult insul inomas. Ann Surg 1990; 212: 615-20
79. Klotter H J, Ruckert K, Kummerle F et al: The use of intraoperative sonography in endocrine tumors of the pancreas. World J Surg 1987; 11: 635-41
80. Krentz A D. Hale P J, Baddeley R M, Williams A C. Natrass M: Intraoperative blood glucose and serum insulin concentrations in (he surgical management of insulinoma. Postgrad Med J 1990; 66: 24-7
81. Fajans S S, Floyd J C Jr, Knopf R F et al: Benzothiadiazine suppression of insulin release from normal and abnormal islet tissue in mano J Clin Invest 1966: 45: 481-5
82. Woltering E, Mozell E. O’Dorisio T et al: Suppression of primary and secondary peptides with somatostatin analog in the therapy 01′ l’unctional endocrine tumors. Surg Gynecol Obstet 1988; 167: 453-7
83. Shaklai M, Aderka D, Blum I et al: Suppression of hypoglycemia altacks and insulin release by propranoloi in a patient with metastatic malignant insulinoma. Diabetes Metab 1977; 3: 155-8
84. Brodows R G, Campbell R G: Control of refractary fasting hypogl icemia in a patient with suspected insulinoma with diphenylhydantoin. J Clin Endocrinol Metab 1974; 38: 159-61
85. Broder L E, Carter S K: Chemotherapy of malignant insulinoma with streptozotocin. In International Congress Series No 314. Amsterdam Exerpta Médica 1974; pp. 714-27
86. Marulanda S: Insulinoma En: Neuroendocrinología quirúrgica. Trabajo para promoción a profesor. U. Na!. 1988; pp. 159-90
87. Langstein H N, Norton J A, Chiang H C V et al: The utility of circulating Icvcls of human pancreatic polypeptide as a marker of islet cell tumors. Surgery
1990; 108: 1109-16
88. Friesen S R: Tumors of the endocrine pancreas. N Engl J Med 1982; 306: 580-90
89. Pipeleers- Marichal M, Willems G et al: Gastrinomas in the duodenums of patients with multiple endocrine neoplasic type 1 and the Zollinger-Ellison syndrome. N Engl J Med 1990; 322: 723-7
90. Grama D, Skoigseid B. Wilander E et al: Pancreatic tumors in multiple endocrine neoplasia type 1: Clinical presentation and surgical treatmen!. World J Surg 1992; 16: 611-8.
![]()