Acalculous Cholecystitis and Covid-19
Acalculous Cholecystitis and Covid-19. A case report
Abstract
Introduction. COVID-19 (Coronavirus disease 2019) is mainly characterized by its respiratory symptoms, but numerous clinical presentations have been described with a recent increment in gastrointestinal manifestations.
Presentation of the case. A 33-year-old, overweight man with no other known medical history, consulted due to symptoms suggestive of biliary pathology and a system review finding of cough and dyspnea. He was taken to surgery due to the finding of AC (Acalculous Cholecystitis) and in the postoperative period, he presented respiratory distress, identifying positive SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus 2), previous idiopathic heart failure, and acute pulmonary thrombosis.
Discussion. The presentation of AC with SARS-CoV-2 is infrequent. It does not have an established clinical pattern and there are multiple confounding factors that make it a diagnostic challenge, and even a distracting factor for the diagnosis of COVID-19 and its complications.
Keywords: Acalculous Cholecystitis; COVID-19; SARS-CoV-2.
Colecistitis Acalculosa y Covid-19. Reporte de caso
Resumen
Introducción. La COVID-19 (del inglés Coronavirus disease 2019), se caracteriza principalmente por su sintomatología respiratoria, pero se han descrito numerosas formas de presentación con un aumento reciente de las manifestaciones gastrointestinales.
Presentación del caso. Varón de 33 años con sobrepeso y sin otros antecedentes conocidos, que consulta por sintomatología sugestiva de patología biliar y hallazgo a la revisión por sistemas de tos y disnea. Es llevado a cirugía por hallazgo de CA (Colecistitis Acalculosa) y en el posoperatorio presenta dificultad respiratoria identificando SARS-CoV-2 (del inglés severe acute respiratory syndrome coronavirus 2) positivo, falla cardíaca idiopática previa y trombosis pulmonar aguda.
Discusión. La presentación de CA con SARS-CoV-2 es infrecuente, no tiene un patrón clínico establecido y sí múltiples factores de confusión que lo tornan en un reto diagnóstico e incluso un factor de distracción para el diagnóstico de la COVID-19 y sus complicaciones.
Palabras clave: Colecistitis Acalculosa; COVID-19; SARS-CoV-2.
Introduction – Acalculous Cholecystitis and Covid-19
To date, COVID-19 produced by the SARS-CoV-2, has reported more than 400 million confirmed cases and more than 5 million deaths around the world according to the latest data from the World Health Organization (1). Although its pathology is mainly characterized by respiratory symptoms, numerous forms of presentation have been described, from mild cutaneous manifestations to severe hematological and cardiac alterations, and other more unusual such as hepatobiliary involvement (2).
AC, defined as a necro-inflammatory state of the gallbladder in the absence of cholelithiasis, occurs more prevalently in critically ill patients, and in those with septic processes. Although AC is well known, it does not have an established clinical pattern, but does have multiple confounding factors that make it a diagnostic challenge (3), as occurred in the following case.
Clinical case – Acalculous Cholecystitis and Covid-19
A 33-year-old, overweight man from Bogotá, with no known medical history and without SARS-CoV-2 vaccination, consulted for 20 days of oppressive pain in the epigastrium radiating to the right hypochondrium, intensity 7/10 and exacerbated by food intake, associated with multiple emetic episodes of food content, increasing on the day of admission. With a system review finding of an eight day dry cough and worsening dyspnea with small exertion.
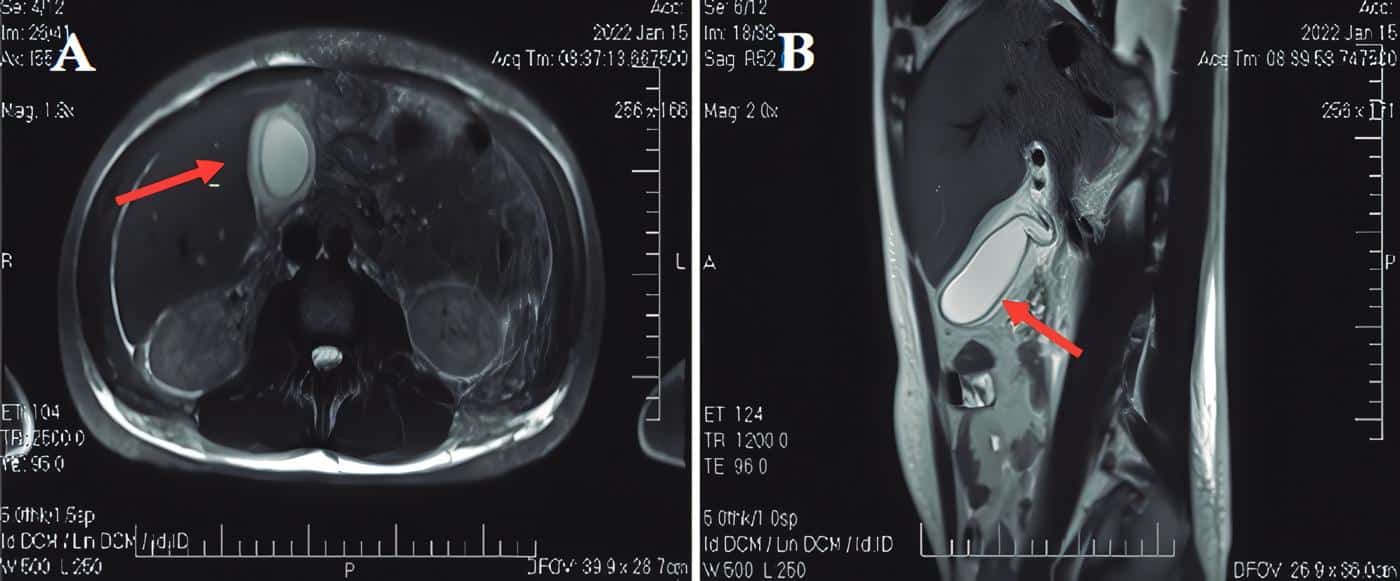
Upon physical examination, he presented normotensive, normal respiratory rate, adequate ambient oxygen saturation, afebrile, mild tachycardia without cardiopulmonary alterations, and soft abdomen with sensation of a painful mass in the right hypochondrium, but without signs of peritoneal irritation. Paraclinical tests showed leukocytosis, direct hyperbilirubinemia, and an alanine aminotransferase-alkaline phosphatase (ALT/ AP) ratio of 0,56 suggestive of cholestasis, but otherwise normal liver profile. The abdominal ultrasound showed a partially distended gallbladder, with thickened walls (9.2 mm), but without endoluminal defects. General Surgery suspected AC with intermediate risk for choledocholithiasis and requested a Magnetic Resonance Cholangiography that showed a distended, stoneless gallbladder with thickened walls (7 mm) and a diagnosis of AC and hepatomegaly (Figure 1).
Figure 1. Magnetic Resonance Cholangiography. A. Axial view in T2. B. Sagittal view in T2. The arrows show the gallbladder with thickened walls, perivesicular fl uid, and no evidence of stones inside.
He was taken to surgery to perform a LapC (Laparoscopic Cholecystectomy) with intraoperative findings of cholecystitis with thickened walls, perivesicular fluid, pericholecystic adhesions, biliary sludge, and congested brown liver.
During the immediate postoperative period, he presented desaturation and bi-basal rales, for which a chest X-ray was requested, showing cardiomegaly, widebased pleural consolidation of the left upper lobe, suggesting pulmonary infarction, with bilateral basal pleural effusion, and RT-PCR (Reverse Transcription polymerase chain reaction) for SARS-CoV-2 positive, glycated hemoglobin in the range of diabetes, and elevated troponin, D-dimer and lactate.
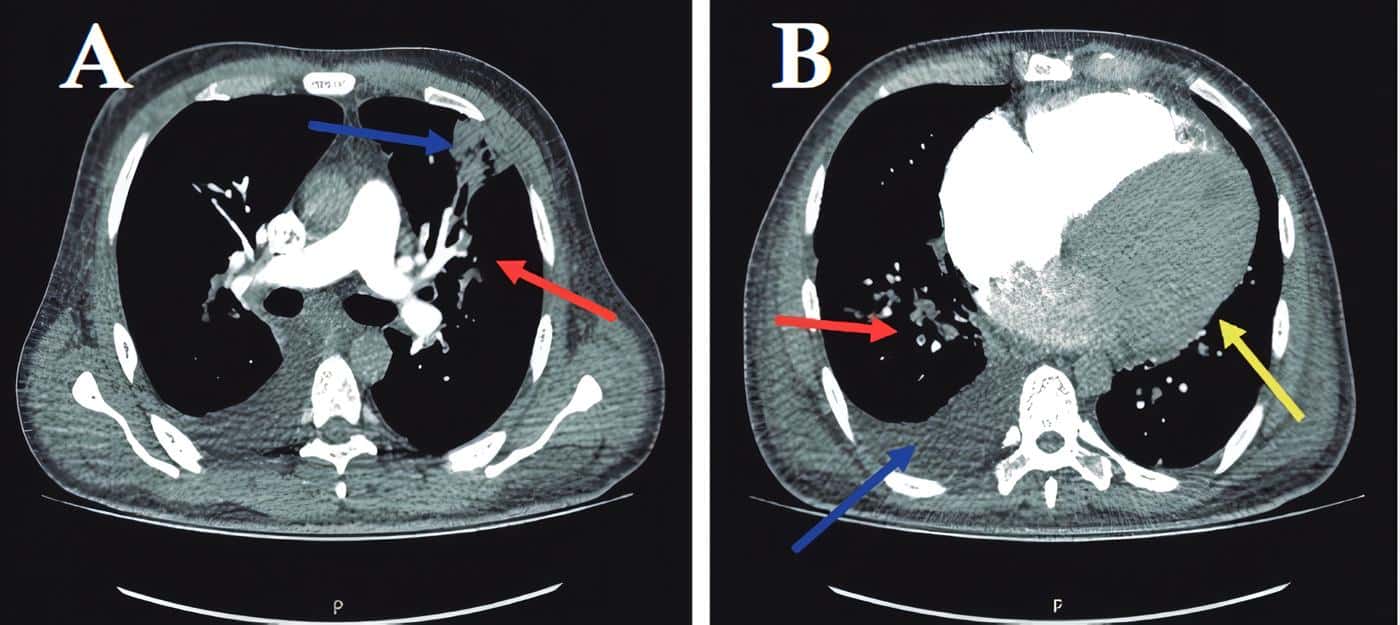
Computed Angio-Tomography of the chest corroborated thrombus and wedge infarction (Figure 2).
Figure 2. Computed angiotomography of the chest with contrast, axial view. A The red arrow shows the location of the central opacifi cation defect, which corresponds to thrombi in the segmental branch for the superior lingular segment, the blue arrow indicates a pleural-based wedge infarction in this same segment. B The red arrow shows the location of the central opacifi cation defect, which corresponds to thrombi in the posterolateral segmental branch of the right lower lobe. The blue arrow shows right pleural eff usion, and the yellow arrow shows cardiomegaly
Management was given with fluids, full anticoagulation, dexamethasone after antiparasitic treatment, and a diagnostic plus evacuatory thoracentesis, which corroborated transudate without malignancy or tuberculosis.
Gallbladder pathology showed velvety mucosa without the presence of stones or tumor-like lesions, with inflammation, muscle hypertrophy, subepithelial histiocytes, Rokitansky sinuses, and serosal congestion.
He required hospitalization in the general ward with oxygen by nasal cannula at 2 liters per minute, and due to adequate evolution, he was discharged after 10 days with anticoagulation, oxygen therapy and oral hypoglycemic agents. Additionally, referral for evaluation by Cardiology due to cardiomegaly in a young patient, where studies concluded idiopathic heart disease with reduced ejection fraction. The patient was then referred to a heart failure clinic, waiting for cardiac transplant.
Discussion – Acalculous Cholecystitis and Covid-19
This case report of a patient with AC and COVID-19, who started with abdominal symptoms prior to respiratory symptoms, shows how not suspecting SARSCoV-2 in patients with predominant abdominal symptoms can delay timely management and diagnosis of its complications, as in this case, a pulmonary thrombotic event.
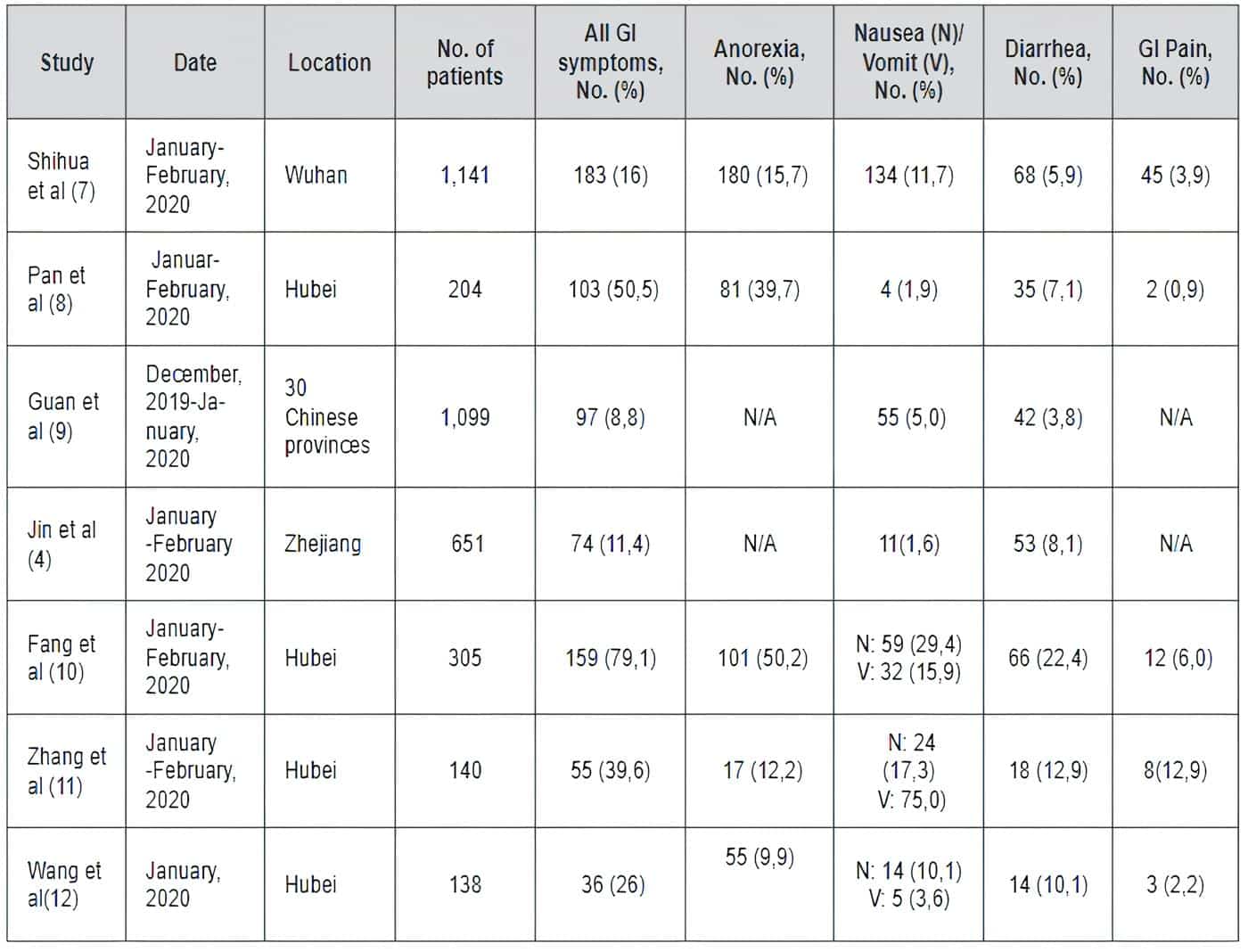
An increase in gastrointestinal symptoms has been seen in patients with COVID-19 even before developing pulmonary manifestations (Table 1) (4-12). This is a difficult case since the presentation of AC with SARS-CoV-2 is infrequent, and less so, in a patient with previous congestive hepatomegaly secondary to unknown idiopathic heart disease, which, because it is painful, can confuse the physician when interpreting suggestive signs of acute hepatobiliary disorder.
Table 1. Gastrointestinal (GI) symptoms associated with COVID-19.
AC represents approximately 10% of all cases of acute cholecystitis and is associated with a high rate of morbi-mortality (3). Various pathological processes have been described that may contribute to its generation. Visceral hypotension and hypoperfusion cause poor and irregular capillary refill of the gallbladder wall, generating ischemia, which could explain a possible association with COVID-19 if it occurs with sepsis (13). The decrease in contractility of the gallbladder muscle generates cholestasis, producing accumulation of bile and increased viscosity, which causes leakage, increased intracholecystic pressure, distention, and increased wall tension. This compromises arterial, lymphatic, and venous flow, leaving it susceptible to infection, gangrene, or total necrosis. Once AC is established, it allows the rapid proliferation of microorganisms, predominantly Escherichia coli, Klebsiella, Bacteroides, Proteus, Pseudomonas, and Enterococcus faecalis (13,14).
The exact pathogenesis of AC in COVID-19 is not clear, but it is known that the intracellular entry of the virus occurs through interaction with the angiotensinconverting enzyme 2 receptor that is present in various tissues- lungs, liver, gallbladder and bile ducts. When SARS-CoV-2 binds, it causes endothelitis which generates thromboembolism in various organs, including the gallbladder. (15,16)
Some publications have tried to demonstrate the relationship between AC and COVID-19.
Yin et al. looked for RT-PCR in the biliary fluid, without detecting it, ruling out that SARS-CoV-2 is eliminated through bile and considering that AC is a complication of SARSCoV-2 (17). In contrast, Balaphas et al. confirmed the presence of virus, by RT-PCR in the gallbladder wall, despite the fact that histological analysis did not show any gallbladder inflammation. The significance of this finding for the pathogenesis of COVID-19 remains to be determined (18).
Futagami et al. carried out a bibliographic search of the published cases of cholestasis related to SARSCoV-2, finding 17 cases (11 men and 6 women); five of them had no comorbidities.
Regarding the onset of cholecystitis, 15 of them developed simultaneously with the diagnosis of pneumonia and two of them later. In case number 5, LapC was performed, and after extubation, he developed respiratory failure, as in the case of our patient. Additionally, at the time of cholecystitis diagnosis, laboratory and imaging findings suggestive of coagulation disorders were confirmed in seven of the cases. Conversely, regarding the initial treatment, emergency cholecystectomy was performed in six patients, and percutaneous drainage in four, of which two failed and were taken to LapC (16).
This suggests that even in patients with AC due to SARSCoV-2, a TOKIO 2018 classification should be performed and emergency cholecystectomy should be considered according to guidelines (19,20).
In conclusion COVID-19 can present only with digestive symptoms, or they can precede the classic respiratory manifestations. AC is one of the less frequent digestive manifestations, but it must be considered even though the pathophysiology in patients with SARS-CoV-2 has not yet been fully clarified. Differential diagnosis can be challenging; therefore, a complete history and physical examination should be systematically performed to reveal a possible positive case, which could make a difference in the patient’s outcome.
Patient Consent – Acalculous Cholecystitis and Covid-19
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editor-in-chief of this journal upon request.
References – Acalculous Cholecystitis and Covid-19
1.WHO Coronavirus (COVID-19) Dashboard. (s. f.). [Internet]. With Vaccination Data. [consultado 14 febrero 2022]. Disponible en:
https://covid19.who.int/#:%7E:text=Globally%2C-as-of-7%3A21pm,5%2C783%2C776-deaths%2C-reported-to-WHO.
2. Gupta, A., Madhavan, M. V., Sehgal, K., Nair, N., Mahajan, S., Sehrawat, T. S.,et al. Extrapulmonary manifestations of COVID-19. Nature Medicine.,2020;26(7):1017–1032.
3. Barie PS, Eachempati SR. Acute acalculous cholecystitis. Gastroenterol Clin North Am . 2010;39(2):343–57.
4. Jin X, Lian J-S, Hu J-H, Gao J, Zheng L, Zhang Y-M, et al. Epidemiological, clinical and virological characteristics of 74 cases of coronavirus-infected disease 2019 (COVID-19) with gastrointestinal symptoms. Gut. 2020;69(6):1002–9.
5. Gavriatopoulou M, Korompoki E, Fotiou D, NtanasisStathopoulos I, Psaltopoulou T, Kastritis E, et al. Organspecific manifestations of COVID-19 infection. Clin Exp Med. 2020;20(4):493–506.
6. Hassani AH, Beheshti A, Almasi F, Ketabi Moghaddam P, Azizi M, Shahrokh S. Unusual gastrointestinal manifestations of COVID-19: two case reports. Gastroenterol Hepatol Bed Bench.2020;13(4):410–4.
7. Luo S, Zhang X, Xu H. Don’t overlook digestive symptoms in patients with 2019 novel Coronavirus disease (COVID-19). Clin Gastroenterol Hepatol. 2020;18(7):1636–7.
Bibliographies – Acalculous Cholecystitis and Covid-19
8. Pan L, Mu M, Yang P, Sun Y, Wang R, Yan J, et al. Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: A descriptive, cross-sectional, multicenter study: A descriptive, cross-sectional, multicenter study. Am J Gastroenterol. 2020;115(5):766– 73.
9. Guan W-J, Ni Z-Y, Hu Y, Liang W-H, Ou C-Q, He J-X, et al. Clinical characteristics of Coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–20.
10. Fang D, Ma JD, Guan JL, et al Manifestations of digestive system of hospitalized patients with coronavirus disease 2019 in Wuhan, China: a single-center descriptive study. Chinese Journal of Digestion.2020;(12):151-156, 2020.
11. Zhang J, Dong X, Cao Y, Yuan Y, Yang Y, Yan Y, et al. Clinical characteristics of 140 patients infected with SARSCoV-2 in Wuhan, China. Allergy. 202075(7):1730-1741.
12. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel Coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–9.
13. McChesney JA, Northup PG, Bickston SJ. Acute acalculous cholecystitis associated with systemic sepsis and visceral arterial hypoperfusion: a case series and review of pathophysiology. Dig Dis Sci. 2003;48(10):1960–7.
14. Wang A-J, Wang T-E, Lin C-C, Lin S-C, Shih S-C. Clinical predictors of severe gallbladder complications in acute acalculous cholecystitis. World J Gastroenterol. [Internet]. 2003;9(12):2821–3.
Recommended Readings – Acalculous Cholecystitis and Covid-19
15. Abaleka FI, Nigussie B, Bedanie G, Mohammed A, Galiboglu S. Acute acalculous cholecystitis due to COVID-19, an unusual presentation. Cureus. 2021;13(6):e15431.
16. Futagami H, Sato H, Yoshida R, Yasui K, Yagi T, Fujiwara T. Acute acalculous cholecystitis caused by SARSCoV-2 infection: A case report and literature review. Int J Surg Case Rep. 2022;90(106731):106731.
17. Ying M, Lu B, Pan J, Lu G, Zhou S, Wang D, et al. COVID-19 with acute cholecystitis: a case report. BMC Infect Dis. 2020;20(1):437.
18. Balaphas A, Gkoufa K, Meyer J, Peloso A, Bornand A, McKee TA, et al. COVID-19 can mimic acute cholecystitis and is associated with the presence of viral RNA in the gallbladder wall. J Hepatol. 2020;73(6):1566–8.
19. Yokoe M, Hata J, Takada T, Strasberg SM, Asbun HJ, Wakabayashi G, et al. Tokyo Guidelines 2018: diagnostic criteria and severity grading of acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci. 2018;25(1):41–54.
20. Okamoto K, Suzuki K, Takada T, Strasberg SM, Asbun HJ, Endo I, et al. Tokyo Guidelines 2018: flowchart for the management of acute cholecystitis. J Hepatobiliary Pancreat Sci. 2018;25(1):55–72.
Authors – Acalculous Cholecystitis and Covid-19
1 Ana María Pérez Murcia. Servicio de Medicina Interna, Hospital de San José. Especialista Docencia Universitaria, Fundación Universitaria de Ciencias de la Salud.
2 Luisa Fernanda Amado. Servicio de Medicina Interna, Hospital de San José. Residente, Fundación Universitaria de Ciencias de la Salud.
3 Laura Camacho. Calidad, Médico Hospitalario. Hospital de San José.
Recibido: 28 de febrero de 2022
Aceptado: 15 de marzo de 2022
Correspondencia:
Ana María Pérez Murcia
mperez1@fucsalud.edu.co
CLIC AQUÍ Y DÉJANOS TU COMENTARIO